Chapter 28: Physical Development in Late Adulthood
Chapter 28 Learning Objectives
- Describe different theories of aging
- Describe the changes in physical appearance in late adulthood
- Describe the sensory changes in late adulthood
- Describe chronic health conditions during late adulthood
- Describe the importance of nutrition and exercise in late adulthood
- Describe the physical and functional changes in the brain during late adulthood
- Explain what happens in Parkison’s disease
- Explain how sleep patterns change in late adulthood
- Explain how sexuality changes in late adulthood
Theories of Aging
Why do we age? There are many theories that attempt to explain how we age, however, researchers still do not fully understand what factors contribute to the human lifespan (Jin, 2010). Research on aging is constantly evolving and includes a variety of studies involving genetics, biochemistry, animal models, and human longitudinal studies (NIA, 2011a). According to Jin (2010), modern biological theories of human aging involve two categories. The first is Programmed Theories that follow a biological timetable, possibly a continuation of childhood development. This timetable would depend on “changes in gene expression that affect the systems responsible for maintenance, repair, and defense responses,” (p. 72). The second category includes Damage or Error Theories which emphasize environmental factors that cause cumulative damage in organisms. Examples from each of these categories will be discussed.
Genetics: One’s genetic make-up certainly plays a role in longevity, but scientists are still attempting to identify which genes are responsible. Based on animal models, some genes promote longer life, while other genes limit longevity. Specifically, longevity may be due to genes that better equip someone to survive a disease. For others, some genes may accelerate the rate of aging, while others decrease the rate. To help determine which genes promote longevity and how they operate, researchers scan the entire genome and compare genetic variants in those who live longer with those who have an average or shorter lifespan. For example, a National Institutes of Health study identified genes possibly associated with blood fat levels and cholesterol, both risk factors for coronary disease and early death (NIA, 2011a).
Researchers believe that it is most likely a combination of many genes that affect the rate of aging.
Evolutionary Theory: Evolutionary psychology emphasizes the importance of natural selection; that is, those genes that allow one to survive and reproduce will be more likely to be transmitted to offspring. Genes associated with aging, such as Alzheimer’s Disease, do not appear until after the individual has passed their main reproductive years. Consequently, natural selection has not eliminated these damaging disorders from the gene pool. If these detrimental disorders occurred earlier in the development cycle, they may have been eliminated already (Gems, 2014).
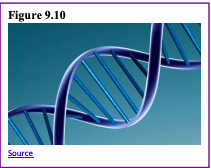
Cellular Clock Theory: This theory suggests that biological aging is due to the fact that normal cells cannot divide indefinitely. This is known as the Hayflick limit and is evidenced in cells studied in test tubes, which divide about 40-60 times before they stop (Bartlett, 2014). But what is the mechanism behind this cellular senescence? At the end of each chromosomal strand is a sequence of DNA that does not code for any particular protein, but protects the rest of the chromosome, which is called a telomere. With each replication, the telomere gets shorter. Once it becomes too short the cell does one of three things. It can stop replicating by turning itself off, called cellular senescence. It can stop replicating by dying, called apoptosis. Or, as in the development of cancer, it can continue to divide and become abnormal. Senescent cells can also create problems. While they may be turned off, they are not dead, thus they still interact with other cells in the body and can lead to an increased risk of disease. When we are young, senescent cells may reduce our risk of serious diseases such as cancer, but as we age they increase our risk of such problems (NIA, 2011a). Understanding why cellular senescence changes from being beneficial to being detrimental are still under investigation. The answer may lead to some important clues about the aging process.
DNA Damage: Over time DNA, which contains the genetic code for all organisms, accumulates damage. This is usually not a concern as our cells are capable of repairing damage throughout our life. Further, some damage is harmless. However, some damage cannot be repaired and remains in our DNA. Scientists believe that this damage, and the body’s inability to fix itself, is an important part of aging (NIA, 2011a). As DNA damage accumulates with increasing age, it can cause cells to deteriorate and malfunction (Jin, 2010). Factors that can damage DNA include ultraviolet radiation, cigarette smoking, and exposure to hydrocarbons, such as auto exhaust and coal (Dollemore, 2006).
Mitochondrial Damage: Damage to mitochondrial DNA can lead to a decaying of the mitochondria, which is a cell organelle that uses oxygen to produce energy from food. The mitochondria convert oxygen to adenosine triphosphate (ATP) which provides the energy for the cell. When damaged, mitochondria become less efficient and generate less energy for the cell and can lead to cellular death (NIA, 2011a).
Free Radicals: When the mitochondria use oxygen to produce energy, they also produce potentially harmful byproducts called oxygen free radicals (NIA, 2011a). The free radicals are missing an electron and create instability in surrounding molecules by taking electrons from them.

There is a snowball effect (A takes from B and then B takes from C, etc.) that creates more free radicals that disrupt the cell and causes it to behave abnormally (See Figure 9.11). Some free radicals are helpful as they can destroy bacteria and other harmful organisms, but for the most part, they cause damage in our cells and tissue. Free radicals are identified with disorders seen in those of advanced age, including cancer, atherosclerosis, cataracts, and neurodegeneration. Some research has supported adding antioxidants to our diets to counter the effects of free radical damage because the antioxidants can donate an electron that can neutralize damaged molecules. However, the research on the effectiveness of antioxidants is not conclusive (Harvard School of Public Health, 2016).
Immune and Hormonal Stress Theories: Ever notice how quickly U.S. presidents seem to age? Before and after photos reveal how stress can play a role in the aging process.

To understand how this stress affects aging, researchers note that both problems with the innate and adaptive immune system play a key role. The innate immune system is made up of the skin, mucous membranes, cough reflex, stomach acid, and specialized cells that alert the body of an impending threat. With age these cells lose their ability to communicate as effectively, making it harder for the body to mobilize its defenses. The adaptive immune system includes the tonsils, spleen, bone marrow, thymus, circulatory system and the lymphatic system that work to produce and transport T cells. T-cells, or lymphocytes, fight bacteria, viruses, and other foreign threats to the body. T-cells are in a “naïve” state before they are programmed to fight an invader and become “memory cells”. These cells now remember how to fight a certain infection should the body ever come across this invader again. Memory cells can remain in your body for many decades, and why the measles vaccine you received as a child is still protecting you from this virus today. As older adults produce fewer new T-cells to be programmed, they are less able to fight off new threats and new vaccines work less effectively. The reason why the shingles vaccine works well with older adults is that they already have some existing memory cells against the varicella virus. The shingles vaccine is acting as a booster (NIA, 2011a).
Hormonal Stress Theory, also known as Neuroendocrine Theory of Aging, suggests that as we age the ability of the hypothalamus to regulate hormones in the body begins to decline to lead to metabolic problems (American Federation of Aging Research (AFAR) 2011). This decline is linked to an excess of the stress hormone cortisol. While many of the body’s hormones decrease with age, cortisol does not (NIH, 2014a). The more stress we experience, the more cortisol released, and the more hypothalamic damage that occurs. Changes in hormones have been linked to several metabolic and hormone-related problems that increase with age, such as diabetes (AFAR, 2011), thyroid problems (NIH, 2013), osteoporosis, and orthostatic hypotension (NIH, 2014a).
Physical Changes of Aging
The Baltimore Longitudinal Study on Aging (BLSA) (NIA, 2011b) began in 1958 and has traced the aging process in 1,400 people from age 20 to 90. Researchers from the BLSA have found that the aging process varies significantly from individual to individual and from one organ system to another. However, some key generalization can be made including:
- Heart muscles thicken with age
- Arteries become less flexible
- Lung capacity diminishes
- Kidneys become less efficient in removing waste from the blood
- Bladder loses its ability to store urine
- Brain cells also lose some functioning, but new neurons can also be produced.
Many of these changes are determined by genetics, lifestyle, and disease. Other changes in late adulthood include:
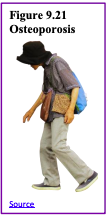
Body Changes: Everyone’s body shape changes naturally as they age. According to the National Library of Medicine (2014) after age 30 people tend to lose lean tissue, and some of the cells of the muscles, liver, kidney, and other organs are lost. Tissue loss reduces the amount of water in your body and bones may lose some of their minerals and become less dense (a condition called osteopenia in the early stages and osteoporosis in the later stages). The amount of body fat goes up steadily after age 30, and older individuals may have almost one third more fat compared to when they were younger. Fat tissue builds up toward the center of the body, including around the internal organs.
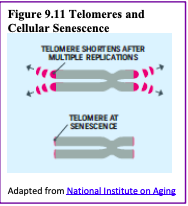
Skin, Hair and Nails: With age skin becomes thinner, less elastic, lose fat, and no longer looks plump and smooth. Veins and bones can be seen easier, and scratches, cuts, and bumps can take longer to heal. Years exposed to the sun may lead to wrinkles, dryness, age spots, and cancer. Older people may bruise more easily, and it can take longer for these bruises to heal. Some medicines or illnesses may also cause bruising. Gravity can cause the skin to sag and wrinkle, and smoking can wrinkle the skin. Also, seen in older adults are age spots, previously called “liver spots”. They look like flat, brown spots and are often caused by years in the sun. Skin tags are small, usually flesh-colored growths of skin that have a raised surface. They become common as people age, especially for women, but both age spots and skin tags are harmless (NIA, 2015f).
Nearly everyone has hair loss as they age, and the rate of hair growth slows down as many hair follicles stop producing new hairs (U.S. National Library of Medicine, 2019). The loss of pigment and subsequent graying begun in middle adulthood continues in late adulthood. The body and face also lose hair. Facial hair may grow coarser. For women, this often occurs around the chin and above the upper lip. For men, the hair of the eyebrows, ears, and nose may grow longer. Nails, particularly toenails, may become hard and thick.
Lengthwise ridges may develop in the fingernails and toenails. However, pits, lines, changes in shape or color should be checked by a healthcare provider as they can be related to nutritional deficiencies or kidney disease (U.S. National Library of Medicine).
Height and Weight: The tendency to become shorter as one age occurs among all races and both sexes. Height loss is related to aging changes in the bones, muscles, and joints. People typically lose almost one-half inch every 10 years after age 40, and height loss is even more rapid after age 70. A total of 1 to 3 inches in height is lost with aging. Changes in body weight vary for men and women. Men often gain weight until about age 55, and then begin to lose weight later in life, possibly related to a drop in the male sex hormone testosterone. Women usually gain weight until age 65, and then begin to lose weight. Weight loss later in life occurs partly because fat replaces lean muscle tissue, and fat weighs less than muscle. Diet and exercise are important factors in weight changes in late adulthood (National Library of Medicine, 2014).
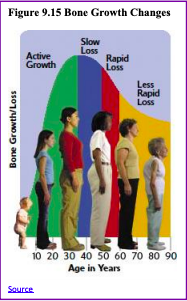
Sarcopenia is the loss of muscle tissue as a natural part of aging. Sarcopenia is most noticeable in men, and physically inactive people can lose as much as 3% to 5% of their muscle mass each decade after age 30, but even when active muscle loss still occurs (Webmd, 2016). Symptoms include a loss of stamina and weakness, which can decrease physical activity and subsequently further shrink muscles. Sarcopenia typically happens faster around age 75, but it may also speed up as early as 65 or as late as 80. Factors involved in sarcopenia include a reduction in nerve cells responsible for sending signals to the muscles from the brain to begin moving, a decrease in the ability to turn protein into energy, and not receiving enough calories or protein to sustain adequate muscle mass. Any loss of muscle is important because it lessens strength and mobility, and sarcopenia is a factor in frailty and the likelihood of falls and fractures in older adults. Maintaining strong leg and heart muscles are important for independence. Weight-lifting, walking, swimming, or engaging in other cardiovascular exercises can help strengthen the muscles and prevent atrophy.
Sensory Changes in Late Adulthood
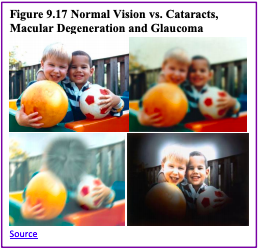
Vision: In late adulthood, all the senses show signs of decline, especially among the oldest-old. In the last chapter, you read about the visual changes that were beginning in middle adulthood, such as presbyopia, dry eyes, and problems seeing in dimmer light. By later adulthood, these changes are much more common. Three serious eye diseases are more common in older adults: Cataracts, macular degeneration, and glaucoma. Only the first can be effectively cured in most people.
Cataracts are a clouding of the lens of the eye. The lens of the eye is made up of mostly water and protein. The protein is precisely arranged to keep the lens clear, but with age, some of the protein starts to clump. As more of the protein clumps together the clarity of the lens is reduced. While some adults in middle adulthood may show signs of cloudiness in the lens, the area affected is usually small enough to not interfere with vision. More people have problems with cataracts after age 60 (NIH, 2014b) and by age 75, 70% of adults will have problems with cataracts (Boyd, 2014). Cataracts also cause a discoloration of the lens, tinting it more yellow and then brown, which can interfere with the ability to distinguish colors such as black, brown, dark blue, or dark purple.
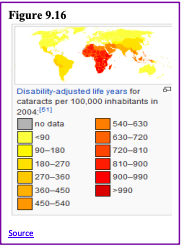
Risk factors besides age include certain health problems such as diabetes, high blood pressure, and obesity, behavioral factors such as smoking, other environmental factors such as prolonged exposure to ultraviolet sunlight, previous trauma to the eye, long-term use of steroid medication, and a family history of cataracts (NEI, 2016a; Boyd, 2014). Cataracts are treated by removing and replacing the lens of the eye with a synthetic lens. In developed countries, such as the United States, cataracts can be easily treated with surgery. However, in developing countries, access to such operations are limited, making cataracts the leading cause of blindness in late adulthood in the least developed countries (Resnikoff, Pascolini, Mariotti & Pokharel, 2004). As shown in Figure 9.16, areas of the world with limited medical treatment for cataracts often results in people living more years with a serious disability. For example, of those living in the darkest red color on the map, more than 990 out of 100,00 people have a shortened lifespan due to the disability caused by cataracts.
Older adults are also more likely to develop age-related macular degeneration, which is the loss of clarity in the center field of vision, due to the deterioration of the macula, the center of the retina. Macular degeneration does not usually cause total vision loss, but the loss of the central field of vision can greatly impair day-to-day functioning. There are two types of macular degeneration: dry and wet. The dry type is the most common form and occurs when tiny pieces of a fatty protein called drusen form beneath the retina. Eventually the macular becomes thinner and stops working properly (Boyd, 2016). About 10% of people with macular degeneration have the wet type, which causes more damage to their central field of vision than the dry form. This form is caused by abnormal development of blood vessels beneath the retina. These vessels may leak fluid or blood causing more rapid loss of vision than the dry form.
The risk factors for macular degeneration include smoking, which doubles your risk (NIH, 2015a); race, as it is more common among Caucasians than African Americans or Hispanics/Latinos; high cholesterol; and a family history of macular degeneration (Boyd, 2016). At least 20 different genes have been related to this eye disease, but there is no simple genetic test to determine your risk, despite claims by some genetic testing companies (NIH, 2015a). At present, there is no effective treatment for the dry type of macular degeneration. Some research suggests that certain patients may benefit from a cocktail of certain antioxidant vitamins and minerals, but the results are mixed at best. They are not a cure for the disease nor will they restore the vision that has been lost. This “cocktail” can slow the progression of visual loss in some people (Boyd, 2016; NIH, 2015a). For the wet type medications that slow the growth of abnormal blood vessels, and surgery, such as laser treatment to destroy the abnormal blood vessels may be used. Only 25% of those with the wet version may see improvement with these procedures (Boyd, 2016).
A third vision problem that increases with age is glaucoma, which is the loss of peripheral vision, frequently due to a buildup of fluid in the eye that damages the optic nerve. As you age the pressure in the eye may increase causing damage to the optic nerve. The exterior of the optic nerve receives input from retinal cells on the periphery, and as glaucoma progresses more and more of the peripheral visual field deteriorates toward the central field of vision. In the advanced stages of glaucoma, a person can lose their sight. Fortunately, glaucoma tends to progress slowly (NEI, 2016b). Glaucoma is the most common cause of blindness in the U.S. (NEI, 2016b). African Americans over age 40 and everyone else over age 60 has a higher risk for glaucoma.
Those with diabetes, and with a family history of glaucoma also have a higher risk (Owsley et al., 2015). There is no cure for glaucoma, but its rate of progression can be slowed, especially with early diagnosis. Routine eye exams to measure eye pressure and examination of the optic nerve can detect both the risk and presence of glaucoma (NEI, 2016b). Those with elevated eye pressure are given medicated eye drops. Reducing eye pressure lowers the risk of developing glaucoma or slow its progression in those who already have it.
Hearing: As you read in Chapter 8, our hearing declines both in terms of the frequencies of sound we can detect, and the intensity of sound needed to hear as we age. These changes continue in late adulthood. Almost 1 in 4 adults aged 65 to 74 and 1 in 2 aged 75 and older have disabling hearing loss (NIH, 2016). Table 9.4 lists some common signs of hearing loss.
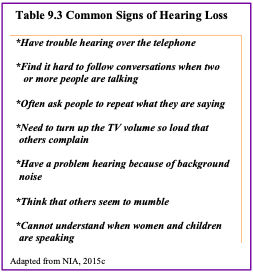
Presbycusis is a common form of hearing loss in late adulthood that results in a gradual loss of hearing. It runs in families and affects hearing in both ears (NIA, 2015c). Older adults may also notice tinnitus, a ringing, hissing, or roaring sound in the ears. The exact cause of tinnitus is unknown, although it can be related to hypertension and allergies. It may come and go or persist and get worse over time (NIA, 2015c). The incidence of both presbycusis and tinnitus increase with age and males have higher rates of both around the world (McCormak, Edmondson-Jones, Somerset, & Hall, 2016).
Your auditory system has two jobs: To help you to hear, and to help you maintain balance. Your balance is controlled by the brain receiving information from the shifting of hair cells in the inner ear about the position and orientation of the body. With age this function of the inner ear declines which can lead to problems with balance when sitting, standing, or moving (Martin, 2014).
Taste and Smell: Our sense of taste and smell are part of our chemical sensing system. Our sense of taste, or gustation, appears to age well. Normal taste occurs when molecules that are released by chewing food stimulate taste buds along with the tongue, the roof of the mouth, and in the lining of the throat. These cells send messages to the brain, where specific tastes are identified. After age 50 we start to lose some of these sensory cells. Most people do not notice any changes in taste until one’s 60s (NIH: Senior Health, 2016b). Given that the loss of taste buds is very gradual, even in late adulthood, many people are often surprised that their loss of taste is most likely the result of a loss of smell.
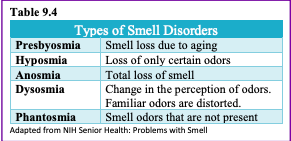
Our sense of smell, or olfaction, decreases more with age, and problems with the sense of smell are more common in men than in women. Almost 1 in 4 males in their 60s have a disorder with the sense of smell, while only 1 in 10 women do (NIH: Senior Health, 2016b). This loss of smell due to aging is called presbyopia. Olfactory cells are located in a small area high in the nasal cavity. These cells are stimulated by two pathways; when we inhale through the nose, or via the connection between the nose and the throat when we chew and digest food. It is a problem with this second pathway that explains why some foods such as chocolate or coffee seem tasteless when we have a head cold. There are several types of loss of smell. Total loss of smell, or anosmia, is extremely rare.
Problems with our chemical senses can be linked to other serious medical conditions such as Parkinson’s, Alzheimer’s, or multiple sclerosis (NIH: Senior Health, 2016a). Any sudden change should be checked out. Loss of smell can change a person’s diet, with either a loss of enjoyment of food and eating too little for balanced nutrition or adding sugar and salt to foods that are becoming blander to the palette.
Touch: Research has found that with age, people may experience reduced or changed sensations of vibration, cold, heat, pressure, or pain (Martin, 2014). Many of these changes are also aligned with a number of medical conditions that are more common among the elderly, such as diabetes. However, there are changes in the touch sensations among healthy older adults. The ability to detect changes in pressure have been shown to decline with age, with it being more pronounced by the 6th decade and diminishing further with advanced age (Bowden & McNelty, 2013). Yet, there is considerable variability, with almost 40% showing sensitivity that is comparable to younger adults (Thornbury & Mistretta, 1981). However, the ability to detect the roughness/smoothness or hardness/softness of an object shows no appreciable change with age (Bowden & McNulty, 2013). Those who show increasing insensitivity to pressure, temperature, or pain are at risk for injury (Martin, 2014).
Pain: According to Molton and Terrill (2014), approximately 60%-75% of people over the age of 65 reports at least some chronic pain, and this rate is even higher for those individuals living in nursing homes. Although the presence of pain increases with age, older adults are less sensitive to pain than younger adults (Harkins, Price, & Martinelli, 1986). Farrell (2012) looked at research studies that included neuroimaging techniques involving older people who were healthy and those who experienced a painful disorder. Results indicated that there were age-related decreases in brain volume in those structures involved in pain. Especially noteworthy were changed in the prefrontal cortex, brainstem, and hippocampus. Women are more likely to identify feeling pain than men (Tsang et al., 2008). Women have fewer opioid receptors in the brain, and women also receive less relief from opiate drugs (Garrett, 2015).

Because pain serves as an important indicator that there is something wrong, a decreased sensitivity to pain in older adults is a concern because it can conceal illnesses or injuries requiring medical attention.
Chronic health problems, including arthritis, cancer, diabetes, joint pain, sciatica, and shingles are responsible for most of the pain felt by older adults (Molton & Terrill, 2014). Cancer is a special concern, especially “breakthrough pain” which is a severe pain that comes on quickly while a patient is already medicated with a long-acting painkiller. It can be very upsetting, and after one attack many people worry it will happen again. Some older individuals worry about developing an addiction to pain medication, but if the medicine is taken exactly as prescribed, addiction should not be a concern (NIH, 2015b). Lastly, side effects from pain medicine including constipation, dry mouth, and drowsiness may occur that can adversely affect the elder’s life.
Some older individuals put off going to the doctor because they think pain is just part of aging and nothing can help. Of course, this is not true. Managing pain is crucial to ensure feelings of well-being for older adults. When chronic pain is not managed, the individual will restrict their movements for fear of feeling pain or injuring themselves further. This lack of activity will result in more restrictions, further decreased participation, and greater disability (Jensen, Moore, Bockow, Ehde, & Engel, 2011). A decline in physical activity because of pain is also associated with weight gain and obesity in adults (Strine, Hootman, Chapman, Okoro, & Balluz, 2005). Additionally, sleep and mood disorders, such as depression, can also occur (Moton & Terrill, 2014). Learning to cope effectively with pain is an important consideration in late adulthood and working with one’s primary physician or a pain specialist is recommended (NIH, 2015b).
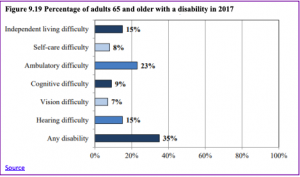
For those 65 and older, 35% have a disability of some type. Figure 9.19 identifies the percentage of those who have a disability based on the type.
Nutrition
A healthy diet is necessary for older adults to increase mental acuteness, resistance to illness and disease, boost energy levels, improve immune system strength, recuperation speed, and have greater effectiveness in the management of chronic health problems (Mayer, 2016). The new MyPlate for Older Adults, a website from Tufts University, suggests that older adults should strive for 50% of their diet is fruits and vegetables; 25% grains, many of which should be whole grains; and 25% protein-rich foods, such as nuts, beans, fish, lean meat, poultry, and fat-free and low-fat dairy products such as milk, cheeses, and yogurts. Unfortunately, changes in sensory functions, such as smell and taste, along with loss of teeth, can derail an older adult’s ability to eat right.

Older adults are likely to use salt and sugar to flavor foods that no longer taste the way they once did. Several government websites provide older adults with alternatives to the salt shaker to make foods more palatable.
Chronic Conditions
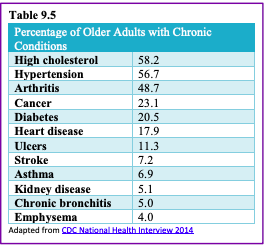
Chronic illnesses are illnesses that are ongoing, generally incurable conditions that require continuous medical attention and affect daily life. As individuals live longer, diseases that affect older individuals will become more prevalent, and the burden of chronic illness grows with age. Less than 50% of adults 50-64 have a chronic condition, 90% aged 75 and up do (Cohen, 2011). Almost 80% have at least one chronic disease, and 77% have at least two (National Council on Aging, 2019). Older women are more likely to have a chronic condition than are older men (83% vs. 88%) (CDC, 2009). Table 9.6 lists the percentage of older adults who have certain chronic illnesses based on the National Health Survey conducted in 2014. Other studies place the figure of diabetes in older adults at 26% (CDC, 2014).
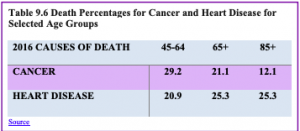
Cancer and Major Cardiovascular Disease: As discussed in chapter 8, cancer and cardiovascular disease are the overall leading causes of death, and they are especially high reasons for death in middle and late adults. Table 9.7 identifies the percentages of deaths due to cancer and cardiovascular disease for selected age groups in 2016; the most recent year for data (Heron, 2018).
Cancer: Advancing age is a significant risk factor for cancer, with persons over 65 accounting for 60% of newly diagnosed cancer and 70% of all cancer deaths (Berger et al., 2006). Additionally, more than 70% of the mortality associated including prostate, bladder, colon, uterus, pancreas, stomach, rectum and lung occurs in patients 65 and older. Other conditions that affect the elderly can occur with cancer, including anemia, coronary artery diseases, congestive heart failure, chronic obstructive pulmonary diseases, renal insufficiency, cerebrovascular diseases, neurovascular complications of diabetes mellitus, and arthritis that restricts mobility (Balducci & Extermann, 2000). Comorbidity will complicate treatment.
Balducci and Extermann (2000) examined several concerns about cancer treatment in the elderly. With aging, there is a decline in multiple organ systems that can adversely affect the ability of medications to treat cancer. Chemotherapy has been found to compromise the cognitive function of those being treated for cancer, and it may further exacerbate dementia and elderly cognitive declines. Frail individuals, defined as having limited life expectancy and near-to- exhausted functional reserves, are also not considered candidates for more toxic forms of chemotherapy. With cancer, the prevalence and risk of malnutrition are higher and diminished visual and hearing function makes elderly cancer patients more susceptible to environmental injury. Screening for depression is also recommended because depression is associated with weight loss, failure to thrive, and may reduce the motivation to receive treatment. Consequently, depression has been associated with decreased survival rates in the elderly. Due to the projected increase in the total number of older patients with cancer, it is recommended that physicians and caretakers have expertise in both oncology and geriatrics (Berger et al., 2006).
Heart Disease: There are changes to the heart that happen with age, and some may increase a person’s risk of heart disease. These include stiffening blood vessels and valves, which may result in leaks or problems pumping blood out of the heart (NIA, 2012). As previously stated, heart disease is the leading cause of death for those in late adulthood (CDC, 2016b). There are different types of heart disease, and as already discussed in chapter 8, the most common is atherosclerosis, the buildup of fatty deposits or plaques in the walls of arteries. As plaque builds up, blood is unable to flow normally and bring oxygen throughout the body, including to the heart. Depending on where the buildup is, atherosclerosis can cause a heart attack, leg pain, or a stroke. However, Atherosclerosis is not part of normal aging. Many of the problems older people have with their heart and blood vessels are caused by disease and not by aging. For example, an older heart can normally pump blood as strong as a younger heart, while less ability to pump blood is caused by disease. Therefore, leading a heart-healthy lifestyle is most important to keeping one’s heart strong in late adulthood.
Arthritis: Arthritis and other rheumatic conditions are the most common cause of disability among US adults and have been the most common cause of disability among US adults for the past 15 years (NIH: National Institute of Arthritis and Musculoskeletal and Skin Diseases, 2014). According to the NIH, approximately 62% of adults with arthritis are 65 years old and up. Almost 1 in 2 older adults with arthritis have some degree of mobility limitations, such as climbing stairs, walking, and grasping objects. The pain and other limitations of arthritis can also increase the risk of depression and other forms of mental distress. Osteoarthritis is the most common type of arthritis. “When the cartilage, the slick, cushioning surface on the ends of bones wears away, bone rubs against bone, causing pain, swelling, and stiffness. Over time, joints can lose strength and pain may become chronic” (Arthritis Foundation, 2017, para 3). Common risk factors for osteoarthritis include genetics, obesity, age, previous injury, and other medical conditions.
Osteoporosis and Kyphosis: Osteoporosis is a disease that thins and weakens bones to the point that they become fragile and break easily. After age 50, 1 in 2 women and 1 in 4 men will experience an osteoporosis-related fracture in their lifetime, often leading to hip, spine, and wrist fractures (Dailey & Cravedi, 2006). Broken hips are a very serious problem as we age. They greatly increase the risk of death, especially during the year after they break (NIH Senior Health, 2015). In the U.S., more than 53 million adults either already have osteoporosis or at high risk due to low bone mass (NIH Senior Health, 2015). As bones weaken in the spine, adults gradually lose height and their posture becomes hunched over, which is called Kyphosis. Over time a bent spine can make it hard to walk or even sit up. Adults can prevent the loss of bone mass by eating a healthy diet with enough calcium and vitamin D, regularly exercising, limiting alcohol, and not smoking (National Osteoporosis Foundation, 2016).
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease in which the airways become damaged making it difficult to breathe. COPD includes problems such as emphysema and chronic bronchitis (NIH Senior Health, 2013). COPD kills more than 120,000 people every year, making it one of the leading causes of death. COPD was once considered a “man’s disease”. However, since 2000, 58% of those with COPD are women and they comprise 8% of all women (American Lung Association, 2019). Research has indicated that women may be more susceptible to the effects of cigarette smoke due to having smaller lungs and estrogen worsening the effects.
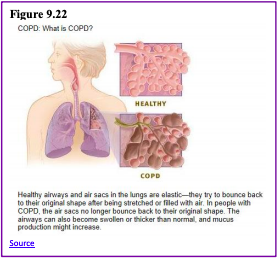
Figure 9.22 compares healthy to damaged lungs due to COPD. As COPD develops slowly, people may not notice the early signs and may attribute the shortness of breath to age or lack of physical exercise. Most people are not diagnosed until midlife or late adulthood. There is no cure as the damage cannot be reversed. Treatments aim at slowing further damage. Cigarette smoking is the leading cause of COPD, but other types of tobacco smoking, such as a pipe or cigar, can cause COPD, especially if the smoke is inhaled. Heavy or long-term exposure to second-hand smoke can also lead to COPD (NIH Senior Health, 2013). COPD can also occur in people who have long term exposure to other environmental irritants, such as chemical fumes, and dust from the environment and workplace.
About 1 in every 1,600 to 5,000 people have a risk for COPD because of a recessive genetic condition known as alpha-1 antitrypsin (AAT) deficiency (NIH, 2011). AAT is a protein made in the liver that protects organs, especially the lungs, from the effects of other harmful proteins. In those with the genetic defect, the AAT protein created is the wrong shape and cannot leave the liver. This can lead to a heightened risk for lung disease, and even liver disease, as the excess of the AAT protein can lead to cirrhosis, which is a disease in which the liver becomes scarred and does not function properly. While some people with ATT deficiency are not affected and live a normal life, COPD is more likely to occur in such individuals if their lungs are exposed to environmental irritants.
Shingles: According to the National Institute on Aging (2015e), the shingle is a disease that affects your nerves. Shingles are caused by the same virus as chickenpox, the varicella-zoster virus (VZV). After you recover from chickenpox, the virus continues to live in some of your nerve cells. It is usually inactive, and most adults live with VZV in their bodies and never get shingles. However, the virus will become active in one in three adults. Instead of causing chickenpox again, it produces shingles. A risk factor for shingles includes advanced age as people have a harder time fighting off infections as they get older. About half of all shingles cases are in adults age 60 or older, and the chance of getting shingles becomes much greater by age 70. Other factors that weaken an individual’s ability to fight infections, such as cancer, HIV infections, or other medical conditions, can put one at a greater risk for developing shingles.
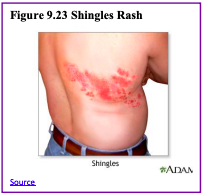
Shingles result in pain, burning, tingling, or itching in the affected area, as well as a rash and blisters. Typically, shingles develop only on one side of the body or face and in a small area rather than all over. Most cases of shingles last 3 to 5 weeks. After the shingles rash goes away, some people may be left with ongoing pain, called post-herpetic neuralgia (PHN) in the area where the rash had been (NIA, 2015e). The older one is when getting shingles, the greater the chance of developing PHN. Some people with PHN find it hard to go about their daily activities, like dressing, cooking and eating. They can also suffer from depression, anxiety, and sleeplessness. Medicines can help with pain and usually, PHN will disappear. Unfortunately, the blisters from shingles may become infected or leave a scar. Blisters near or in the eye can cause lasting eye damage or blindness. A brief paralysis of the face, hearing loss, and very rarely, swelling of the brain (encephalitis) can also occur. There is a shingles vaccine that is recommended for those aged 50 and older. Shingles are not contagious, but one can catch chickenpox from someone with shingles.
Beliefs about Health: Despite the fact that the majority of older adults have at least one chronic illness, most rate their overall health positively (Graham, 2019). Based on the results of the CDC’s 2017 National Health Interview Survey, 82% of those aged 65-74 and 73% of those 75 and older rated their health as excellent, very good or good. Because older adults focus more on emotional well-being, positive social relationships, remaining active, and overall life satisfaction, poor physical functioning is not considered as important. Older adults often look to those who are worse off than themselves, including those having died or are in a nursing home, and consequently feel more positive about themselves. This perspective is in contrast to those younger who believe that there should not be anything wrong with them, and consequently experience negative feelings when they have an illness. Older adults expect there will be some deterioration in their health and are able to adapt to it. Similarly, most older adults identify positive mental health in conjunction with their physical health.
Brain Functioning
Research has demonstrated that the brain loses 5% to 10% of its weight between 20 and 90 years of age (Fjell & Walhovd, 2010). This decrease in brain volume appears to be due to the shrinkage of neurons, lower number of synapses, and shorter length of axons. According to Garrett (2015), the normal decline in cognitive ability throughout the lifespan has been associated with brain changes, including the reduced activity of genes involved in memory storage, synaptic pruning, plasticity, and glutamate and GABA (neurotransmitters) receptors. There is also a loss in white matter connections between brain areas. Without myelin, neurons demonstrate slower conduction and impede each other’s actions. A loss of synapses occurs in specific brain areas, including the hippocampus (involved in memory) and the basal forebrain region. Older individuals also activate larger regions of their attentional and executive networks, located in the parietal and prefrontal cortex, when they perform complex tasks. This increased activation correlates with reduced performance on both executive tasks and tests of working memory when compared to those younger (Kolb & Whishaw, 2011).
Continued Neurogenesis: Researchers at the University of Chicago found that new neurons continued to form into old age. Tobin et al. (2019) examined the post-mortem brain tissue of individuals between the ages of 79 and 99 (average age 90.6) and found evidence of neurogenesis in the hippocampus. Approximately 2000 neural progenitor cells and 150, 000 developing neurons were found per brain, although the number of developing neurons was lower in people with cognitive impairments or Alzheimer’s disease. Tobin et al. hypothesized that the lower levels of neurogenesis in the hippocampus were associated with symptoms of cognitive decline and reduced synaptic plasticity.
The brain in late adulthood also exhibits considerable plasticity, and through practice and training, the brain can be modified to compensate for any age-related changes (Erber & Szuchman, 2015). Park and Reuter-Lorenz (2009) proposed the Scaffolding Theory of Aging and Cognition which states that the brain adapts to neural atrophy (dying of brain cells) by building alternative connections, referred to as scaffolding. This scaffolding allows older brains to retain high levels of performance. Brain compensation is especially noted in the additional neural effort demonstrated by those individuals who are aging well. For example, older adults who performed just as well as younger adults on a memory task used both prefrontal areas, while only the right prefrontal cortex was used in younger participants (Cabeza, Anderson, Locantore, & McIntosh, 2002). Consequently, this decrease in brain lateralization appears to assist older adults with their cognitive skills.
Healthy Brain Functioning: Cheng (2016) found that physical activity and stimulating cognitive activity resulted in significant reductions in the risk of neurocognitive disorders in longitudinal studies. Physical activity, especially aerobic exercise, is associated with less age-related gray and white matter loss, as well and diminished neurotoxins in the brain. Overall, physical activity preserves the integrity of neurons and brain volume. Cognitive training improves the efficiency of the prefrontal cortex and executive functions, such as working memory, and strengthens the plasticity of neural circuits. Both activities support cognitive reserve, or “the structural and dynamic capacities of the brain that buffer against atrophies and lesions” (p. 85). Although it is optimal to begin physical and cognitive activities earlier in life, it is not too late to start these programs in late adulthood to improve one’s cognitive health.

Can we improve brain functioning? Many training programs have been created to improve brain functioning. ACTIVE (Advanced Cognitive Training for Independent and Vital Elderly), a study conducted between 1999 and 2001 in which 2,802 individuals age 65 to 94, suggests that the answer is “yes”. These racially diverse participants received 10 group training sessions and 4 follow up sessions to work on tasks of memory, reasoning, and speed of processing. These mental workouts improved cognitive functioning even 5 years later. Many of the participants believed that this improvement could be seen in everyday tasks as well (Tennstedt et al., 2006). However, programs for the elderly on memory, reading, and processing speed training demonstrate that there is an improvement in the specific tasks trained, but there is no generalization to other abilities (Jarrett, 2015). Further, these programs have not been shown to delay or slow the progression of Alzheimer’s disease. Although these programs are not harmful, “physical exercise, learning new skills, and socializing remain the most effective ways to train your brain” (p. 207). These activities appear to build a reserve to minimize the effects of primary aging of the brain.
Parkinson’s disease is characterized by motor tremors, loss of balance, poor coordination, rigidity, and difficulty moving (Garrett, 2015). Parkinson’s affects approximately 1% of those over the age of 60, and it appears more frequently in family members in a little less than 10% of cases. Twenty-eight chromosomal areas have been implicated in Parkinson’s disease, but environmental factors have also been identified and include brain injury. Being knocked unconscious once increases the risk by 32% and being knocked out several times increases the risk by 174% (Garrett, 2015). Other environmental influences include toxins, industrial chemicals, carbon monoxide, herbicides and pesticides (Olanow & Tatton, 1999). The symptoms are due to the deterioration of the substantia nigra, an area in the midbrain whose neurons send dopamine-releasing axons to the basal ganglia which affect motor activity. Treatment typically includes the medication levodopa (L-dopa), which crosses the blood-brain barrier and is converted into dopamine in the brain. Deep brain stimulation, which involves inserting an electrode into the brain that provides electrical stimulation, has resulted in improved motor functioning (Garrett, 2015).
Sleep
Similar to other adults, older adults need between 7 to 9 hours of sleep per night, but they tend to go to sleep earlier and get up earlier than those younger. This pattern is called advanced sleep phase syndrome and is based on changes in circadian rhythms (National Sleep Foundation, 2009). There are sleep problems in older adults, and insomnia is the most common problem in those 60 and older (NIA, 2016). People with insomnia have trouble falling asleep and staying asleep. There are many reasons why older people may have insomnia, including certain medications, being in pain, having a medical or psychiatric condition, and even worrying before bedtime about not being able to sleep. Using over the counter sleep aids or medication may only work when used for a short time. Consequently, sleep problems should be discussed with a health care professional.
Also, common in older adults are sleep disorders, including sleep apnea, restless legs syndrome, periodic limb movement disorder, and rapid eye movement sleep behavior disorder (NIA, 2016). Sleep apnea refers to repeated short pauses in breathing, while an individual sleeps, which can lead to reduced oxygen in the blood. Snoring is a common symptom of sleep apnea and it often worsens with age. Untreated sleep apnea can lead to impaired daytime functioning, high blood pressure, headaches, stroke, and memory loss. Restless legs syndrome feels like there is tingling, crawling, or pins and needles in one or both legs, and this feeling is worse at night.
Periodic limb movement disorder causes people to jerk and kick their legs every 20 to 40 seconds during sleep. Rapid eye movement sleep behavior disorder occurs when one’s muscles can move during REM sleep and sleep is disrupted.
According to the National Sleep Foundation (2009), there are many medical conditions that affect sleep and include gastroesophageal reflux disease, diabetes mellitus, renal failure, respiratory diseases such as asthma, and immune disorders. Diseases such as Parkinson’s disease and multiple sclerosis also commonly cause problems sleeping. Lastly, Alzheimer’s disease can interfere with sleeping patterns. Individuals may wake up many times during the night, wander when up, and yell which can alter the amount of time they sleep. Both minor and major sleep problems in older adults can lead to increased risk of accidents, falls, chronic fatigue, decreased quality of life, cognitive decline, reduced immune function, and depression (Buman, 2013).

Sexuality
Because of sleep problems experienced by those in late adulthood, research has looked into whether exercise can improve their quality of sleep. Results show that 150 minutes per week of exercise can improve sleep quality (Buman, 2013). This amount of exercise is also recommended to improve other health areas including lowering the risk for heart disease, diabetes, and some cancers. Aerobic activity, weight training, and balance programs are all recommended. For those who live in assisted living facilities even light exercise, such as stretching and short walks, can improve sleep. High-intensity activity is not necessary to see improvements. Overall, the effects of exercise on sleep may actually be even larger for older adults since their sleep quality may not be ideal to start.
According to Kane (2008), older men and women are often viewed as genderless and asexual. There is a stereotype that elderly individuals no longer engage in sexual activity and when they do, they are perceived to have committed some kind of offense. These ageist myths can become internalized, and older people have a more difficult time accepting their sexuality (Gosney, 2011). Additionally, some older women indicate that they no longer worry about sexual concerns anymore once they are past the childbearing years.
In reality, many older couples find greater satisfaction in their sex life than they did when they were younger. They have fewer distractions, more time and privacy, no worries about getting pregnant, and greater intimacy with a lifelong partner (NIA, 2013). Results from the National Social Life Health, and Aging Project indicated that 72% of men and 45.5% of women aged 52 to 72 reported being sexually active (Karraker, DeLamater, & Schwarz, 2011). Additionally, the National Survey of Sexual Health data indicated that 20%-30% of individuals remain sexually active well into their 80s (Schick et al., 2010). However, there are issues that occur in older adults that can adversely affect their enjoyment of healthy sexual relationships.
Causes of Sexual Problems: According to the National Institute on Aging (2013), chronic illnesses including arthritis (joint pain), diabetes (erectile dysfunction), heart disease (difficulty achieving orgasm for both sexes), stroke (paralysis), and dementia (inappropriate sexual behavior) can all adversely affect sexual functioning. Hormonal changes, physical disabilities, surgeries, and medicines can also affect a senior’s ability to participate in and enjoy sex. How one feels about sex can also affect performance. For example, a woman who is unhappy about her appearance as she ages may think her partner will no longer find her attractive. A focus on youthful physical beauty for women may get in the way of her enjoyment of sex. Likewise, most men have a problem with erectile dysfunction (ED) once in a while, and some may fear that ED will become a more common problem as they age. If there is a decline in sexual activity for a heterosexual couple, it is typically due to a decline in the male’s physical health (Erber & Szuchman, 2015).
Overall, the best way to experience a healthy sex life in later life is to keep sexually active while aging. However, the lack of an available partner can affect heterosexual women’s participation in a sexual relationship. Beginning at age 40 there are more women than men in the population, and the ratio becomes 2 to 1 at age 85 (Karraker et al., 2011). Because older men tend to pair with younger women when they become widowed or divorced, this also decreases the pool of available men for older women (Erber & Szuchman, 2015). In fact, a change in marital status does not result in a decline in the sexual behavior of men aged 57 to 85 years old, but it does result in a decline for similar-aged women (Karraker et al., 2011).
Concluding Thoughts: Key players in improving the quality of life among older adults will be those adults themselves. By exercising, reducing stress, stopping smoking, limiting the use of alcohol, and consuming more fruits and vegetables, older adults can expect to live longer and more active lives (He et al., 2005). Stress reduction, both in late adulthood and earlier in life, is also crucial. The reduction of societal stressors can promote active life expectancy. In the last 40 years, smoking rates have decreased, but obesity has increased, and physical activity has only modestly increased.
References
Acierno, R., Hernandez, M. A., Amstadter, A. B., Resnick, H. S., Steve, K., Muzzy, W., & Kilpatrick, D. G. (2010). Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: The National Elder Mistreatment Study. American Journal of Public Health, 100, 292-297.
Administration on Aging. (2017). 2017 Profile of older Americans. Retrieved from: https://acl.gov/sites/default/files/Aging%20and%20Disability%20in%20America/2017OlderAmericansProfile.pdf
Alleccia, J., & Bailey, M. (2019, June 12). A concern for LGBT boomers. The Chicago Tribune, pp. 1-2.
Alterovitz, S. S., & Mendelsohn, G. A. (2011). Partner preferences across the lifespan: Online dating by older adults. Psychology of Popular Media Culture, 1, 89-95.
Alzheimer’s Association. (2016). Know the 10 signs. Early detection matters. Retrieved from: http://www.alz.org/national/documents/tenwarnsigns.pdf
American Federation of Aging Research. (2011). Theories of aging. Retrieved from http://www.afar.org/docs/migrated/111121_INFOAGING_GUIDE_THEORIES_OF_AGINGFR.pdf
American Heart Association. (2014). Overweight in children. Retrieved from http://www.heart.org/HEARTORG/HealthyLiving/HealthyKids/ChildhoodObesity/Overweight-in- Children_UCM_304054_Article.jsp#.V5EIlPkrLIU
American Lung Association. (2018). Taking her breath away: The rise of COPD in women. Retrieved from https://www.lung.org/assets/documents/research/rise-of-copd-in-women-full.pdf
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington, DC: Author.
American Psychological Association. (2016). Older adults’ health and age-related changes. Retrieved from http://www.apa.org/pi/aging/resources/guides/older.aspx
Andrés, P., Van der Linden, M., & Parmentier, F. B. R. (2004). Directed forgetting in working memory: Age-related differences. Memory, 12, 248-256.
Antonucci, T. C. (2001). Social relations: An examination of social networks, social support and sense of control. In J.E. Birren & K. W. Schaie (Eds.), Handbook of the psychology of aging (5th ed., pp. 427–453). New York: Academic Press.
Arias, E., & Xu, J. (2019). United States life tables, 2017. National Vital Statistics Reports, 68(7), 1-66.
Arthritis Foundation. (2017). What is arthritis? Retrieved from http://www.arthritis.org/about-arthritis/understanding- arthritis/what-is-arthritis.php
Ash, A. S., Kroll-Desroisers, A. R., Hoaglin, D. C., Christensen, K., Fang, H., & Perls, T. T. (2015). Are members of long-lived families healthier than their equally long-lived peers? Evidence from the long life family study. Journal of Gerontology: Series A: Biological Sciences and Medical Sciences. Advance online publication. doi:10.1093/gerona/glv015
Atchley, R. C. (1994). Social forces and aging (7th ed.). Belmont, CA: Wadsworth.
Balducci, L., & Extermann, M. (2000). Management of cancer if the older person: A practical approach. The Oncologist. Retrieved from http://theoncologist.alphamedpress.org/content/5/3/224.full
Baltes, B. B., & Dickson, M. W. (2001). Using life-span models in industrial/organizational psychology: The theory of selective optimization with compensation (soc). Applied Developmental Science, 5, 51-62.
Baltes, P. B. (1993). The aging mind: Potential and limits. The Gerontologist, 33, 580-594.
Baltes, P.B. & Kunzmann, U. (2004). The two faces of wisdom: Wisdom as a general theory of knowledge and judgment about excellence in mind and virtue vs. wisdom as everyday realization in people and products. Human Development, 47(5), 290-299.
Baltes, P. B. & Lindenberger, U. (1997). Emergence of powerful connection between sensory and cognitive functions across the adult life span: A new window to the study of cognitive aging? Psychology and Aging, 12, 12–21.
Baltes, P. B., & Staudinger, U. M. (2000). Wisdom: A metaheuristic (pragmatic) to orchestrate mind and virtue toward excellence. American Psychologist, 55 (1), 122-136.
Barker, (2016). Psychology for nursing and healthcare professionals. Thousand Oaks, CA: Sage.
Barnes, S. F. (2011a). Fourth age-the final years of adulthood. San Diego State University Interwork Institute. Retrieved from http://calbooming.sdsu.edu/documents/TheFourthAge.pdf
Barnes, S. F. (2011b). Third age-the golden years of adulthood. San Diego State University Interwork Institute. Retrieved from http://calbooming.sdsu.edu/documents/TheThirdAge.pdf
Bartlett, Z. (2014). The Hayflick limit. Embryo Project Encyclopedia. Retrieved from http://embryo.asu.edu/handle/10776/8237
Bennett, K. M., Hughes, G. M., & Smith, P. T. (2005). Psychological response to later life widowhood: Coping and the effects of gender. Omega, 51, 33-52.
Benson, J.J., & Coleman, M. (2016). Older adults developing a preference for living apart together. Journal of Marriage and Family, 18, 797-812.
Berger, N. A., Savvides, P., Koroukian, S. M., Kahana, E. F., Deimling, G. T., Rose, J. H., Bowman, K. F., & Miller, R. H. (2006). Cancer in the elderly. Transactions of the American Clinical and Climatological Association, 117, 147-156.
Berk, L. (2007). Development through the life span (4th ed.). Boston: Allyn and Bacon.
Blanchard-Fields, F. (2007). Everyday problem solving and emotion: An adult development perspective. Current Directions in Psychoogical Science, 16, 26–31
Blank, T. O. (2005). Gay men and prostate cancer: Invisible diversity. American Society of Clinical Oncology, 23, 2593–2596. doi:10.1200/ JCO.2005.00.968
Blazer, D. G., & Wu, L. (2009). The epidemiology of substance use and disorders among middle aged and elderly community adults: National Survey on Drug Use and Health. American Journal of Geriatric Psychiatry, 17, 237-245.
Bookwala, J., Marshall, K. I., & Manning, S. W. (2014). Who needs a friend? Marital status transitions and physical health outcomes in later life. Health Psychology, 33(6), 505-515.
Borysławski, K., & Chmielewski, P. (2012). A prescription for healthy aging. In: A Kobylarek (Ed.), Aging: Psychological, biological and social dimensions (pp. 33-40). Wrocław: Agencja Wydawnicza.
Botwinick, J. (1984). Aging and behavior (3rd ed.). New York: Springer.
Bowden, J. L., & McNulty, P. A. (2013). Age-related changes in cutaneous sensation in the healthy human hand. Age (Dordrecht, Netherlannds), 35(4), 1077-1089.
Boyd, K. (2014). What are cataracts? American Academy of Ophthalmology. Retrieved from http://www.aao.org/eye- health/diseases/what-are-cataracts
Boyd, K. (2016). What is macular degeneration? American Academy of Ophthalmology. Retrieved from http://www.aao.org/eye-health/diseases/amd-macular-degeneration
Brehm, S. S., Miller, R., Perlman, D., & Campbell, S. (2002). Intimate relationships (3rd ed.). Boston: McGraw-Hill Higher Education.
Buman, M. P. (2013). Does exercise help sleep in the elderly? Retrieved from https://sleepfoundation.org/ask-the-expert/does-exercise-help-sleep-the-elderly
Cabeza, R., Anderson, N. D., Locantore, J. K., & McIntosh, A. R. (2002). Aging gracefully: Compensatory brain activity in high- performing older adults. NeuroImage, 17, 1394-1402.
Carlson, N. R. (2011). Foundations of behavioral neuroscience (8th ed.). Boston, MA: Pearson Education.
Carr, D. (2004a). The desire to date and remarry among older widows and widowers. Journal of Marriage and Family, 66, 1051– 1068.
Carr, D. (2004b). Gender, preloss marital dependence, and older adults’ adjustment to widowhood. Journal of Marriage and Family, 66, 220-235.
Carstensen, L. L. (1993). Motivation for social contact across the life span: A theory of socioemotional selectivity. In J. E. Jacobs (Ed.), Nebraska Symposium on Motivation, 1992: Developmental perspectives on motivation (pp. 209–254). Lincoln, NE: University of Nebraska Press.
Carstenson, L. L., Fung, H. H., & Charles, S. T. (2003). Socioemotional selectivity theory and the regulation of emotion in the second half of life. Motivation and Emotion, 27, 103-123.
Carstensen, L. L., Gottman, J. M., & Levensen, R. W. (1995). Emotional behavior in long-term marriage. Psychology and Aging, 10, 140–149.
Carstensen, L. L., Isaacowitz, D. M., & Charles, S. T. (1999). Taking time seriously: A theory of socioemotional selectivity. American Psychologist, 54, 165–181.
Caruso, C., Accardi, G., Virruso, C., & Candore, G. (2013). Sex, gender and immunosenescence: A key to understand the different lifespan between men and women? Immunity & Ageing, 10, 20.
Centers for Disease Control and Prevention. (2008). Persons age 50 and over: Centers for disease control and prevention. Atlanta, GA: Author.
Centers for Disease Control and Prevention. (2009). Percent of U. S. adults 55 and over with chronic conditions. Retrieved from http://www.cdc.gov/nchs/health_policy/adult_chronic_conditions.htm
Centers for Disease Control and Prevention. (2011). Rationale for regular reporting on health disparities and inequalities—United States. Morbidity and Mortality Weekly Report, 60, 3–10.
Centers for Disease Control and Prevention. (2013). State-Specific Healthy Life Expectancy at Age 65 Years — United States, 2007–2009. Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6228a1.htm
Centers for Disease Control and Prevention. (2014). National Diabetes Statistics Report, 2014. Retrieved from http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf
Centers for Disease Control and Prevention. (2016a). Increase in Suicide in the United States, 1999–2014. Retrieved from http://www.cdc.gov/nchs/products/databriefs/db241.htm
Centers for Disease Control and Prevention. (2016b). Older Persons’ Health. Retrieved from http://www.cdc.gov/nchs/fastats/older-american-health.htm
Central Intelligence Agency. (2019). The world factbook. Retrieved from https://www.cia.gov/library/publications/the-world- factbook/fields/355rank.html
Charness, N. (1981). Search in chess: Age and skill differences. Journal of Experimental Psychology: Human Perception and Performance, 7, 467.
Cheng, S. (2016). Cognitive reserve and the prevention of dementia: The role of physical and cognitive activities. Current Psychiatry Reports, 18(9), 85.
Chmielewski, P., Boryslawski, K., & Strzelec, B. (2016). Contemporary views on human aging and longevity. Anthropological Review, 79(2), 115-142.
Cohen, D., & Eisdorfer, C. (2011). Integrated textbook of geriatric mental health. Baltimore: Johns Hopkins University Press. Cohen, R. M. (2011). Chronic disease: The invisible illness. AARP. Retrieved from http://www.aarp.org/health/conditions-treatments/info-06-2011/chronic-disease-invisible-illness.html
Cohn, D., & Passel, J. (2018). A record 64 million Americans live in multigenerational households. Retrieved from https://www.pewresearch.org/fact-tank/2018/04/05/a-record-64-million-americans-live-in-multigenerational- households/
Craik, F. I., & Bialystok, E. (2006). Cognition through the lifespan: mechanisms of change. Trends in Cognitive Sciences, 10, 131–138.
Dahlgren, D. J. (1998). Impact of knowledge and age on tip-of-the-tongue rates. Experimental Aging Research, 24, 139-153. Dailey, S., & Cravedi, K. (2006). Osteoporosis information easily accessible NIH senior health. National Institute on Aging. Retrieved from https://www.nia.nih.gov/newsroom/2006/01/osteoporosis-information-easily-accessible-nihseniorhealth
David, S., & Knight, B. G. (2008). Stress and coping among gay men: Age and ethnic differences. Psychology and Aging, 23, 62– 69. doi:10.1037/ 0882-7974.23.1.62
Davidson, K. (2001). Late life widowhood, selfishness and new partnership choices: A gendered perspective. Ageing and Society, 21, 297–317.
Department of Defense. (2015). Defense advisory committee on women in the services. Retrieved from http://dacowits.defense.gov/Portals/48/Documents/Reports/2015/Annual%20Report/2015%20DACOWITS%20Annual%20Report_Final.pdf
de Vries, B. (1996). The understanding of friendship: An adult life course perspective. In C. Magai & S. H. McFadden (Eds.), Handbook of emotion, adult development, and aging (pp. 249–268). San Diego, CA: Academic Press.
DiGiacomo, R. (2015). Road scholar, once elderhostel, targets boomers. Retrieved from https://www.forbes.com/sites/nextavenue/2015/10/05/road-scholar-once-elderhostel-targets-boomers/#fcb4f5b64449
Dixon R. A., & Cohen, A. L. (2003). Cognitive development in adulthood. In R. M. Lerner, M. A. Easterbrokks & J. Misty (Eds.), Handbook of psychology (pp. 443-461). Hoboken NJ: John Wiley.
Dixon, R. A., Rust, T. B., Feltmate, S. E., & See, S. K. (2007). Memory and aging: Selected research directions and application issues. Canadian Psychology, 48, 67-76.
Dollemore, D. (2006, August 29). Publications. National Institute on Aging. Retrieved from http://www.nia.nih.gov/HealthInformation/Publications?AgingUndertheMicroscope/
Economic Policy Institute. (2013). Financial security of elderly Americans at risk. Retrieved from http://www.epi.org/publication/economic-security-elderly-americans-risk
Elwert, F., & Christakis, N. (2008). The effect of widowhood on mortality by the causes of death of both spouses. American Journal of Public Health, 98, 2092-2098.
Erber, J. T., & Szuchman, L. T. (2015). Great myths of aging. West Sussex, UK: John Wiley & Sons. Erikson, E. H. (1982). The life cycle completed. New York, NY: Norton & Company.
Farrell, M. J. (2012). Age-related changes in the structure and function of brain regions involved in pain processing. Pain Medication, 2, S37-43. doi: 10.1111/j.1526-4637.2011.01287.x.
Federal Bureau of Investigation.üü (2014). Crime in the United States. Retrieved from https://ucr.fbi.gov/crime-in-the- u.s/2014/crime-in-the-u.s.-2014/tables/expanded- homicide- data/expanded_homicide_data_table_1_murder_victims_by_race_ethnicity_and_sex_2014.xls
Fingerman, K. L., & Birditt, K. S. (2011). Relationships between adults and their aging parents. In K. W. Schaie & S. I Willis (Eds.). Handbook of the psychology of aging (7th ed.) (pp 219-232). SanDiego: Elsevier Academic Press.
Fischer, C. S. (1982). To dwell among friends: Personal networks in town and city. Chicago, IL: University of Chicago Press.
Fjell, A. M., & Walhovd, K. B. (2010). Structural brain changes in aging: Courses, causes, and cognitive consequences. Reviews in the Neurosciences, 21, 187-222.
Fox, S. (2004). Older Americans and the Internet. PEW Internet & American Life Project. Retrieved from http://www.pewinternet.org/report_display.asp?r_117
Fredriksen-Goldsen, K. I., Kim, H. J., Emlet, C. A., Muraco, A., Erosheva, E. A., Hoy-Ellis, C. P.,… Petry, H. (2011). The aging and health report: disparities and resilience among lesbian, gay, bisexual, and transgender older adults. Seattle, WA: Institute for Multigenerational Health.
Garrett, B. (2015). Brain and behavior (4th ed.) Thousand Oaks, CA: Sage.
Gatz, M., Smyer, M. A., & DiGilio, D. A. (2016). Psychology’s contribution to the well-being of older Americans. American Psychologist, 71(4), 257-267.
Gems, D. (2014). Evolution of sexually dimorphic longevity in humans. Aging, 6, 84-91.
George, L.K. (2009). Still happy after all these years: research frontiers on subjective well-being in later life. Journal of Gerontology: Social Sciences, 65B (3), 331–339. doi:10.1093/geronb/gbq006
Githens, K., & Abramsohn, E. (2010). Still got it at seventy: Sexuality, aging, and HIV. Achieve, 1, 3-5.
Glaser, K., Stuchbury, R., Tomassini, C., & Askham, J. (2008). The long-term consequences of partnership dissolution for support in later life in the Unites Kingdom. Ageing & Society, 28(3), 329-351.
Gosney, T. A. (2011). Sexuality in older age: Essential considerations for healthcare professionals. Age Ageing, 40(5), 538-543. Göthe, K., Oberauer, K., & Kliegl, R. (2007). Age differences in dual-task performance after practice. Psychology and Aging, 22, 596-606.
Goyer, A. (2010). More grandparents raising grandkids: New census data shows and increase in children being raised by extended family. AARP. Retrieved from http://www.aarp.org/relationships/grandparenting/info-12- 2010/more_grandparents_raising_grandchildren.html
Graham, J. (2019, July 10). Why many seniors rate their health positively. The Chicago Tribune, p. 2.
Greenfield, E. A., Vaillant, G. E., & Marks, N. F. (2009). Do formal religious participation and spiritual perceptions have independent linkages with diverse dimensions of psychological well-being? Journal of Health and Social Behavior, 50, 196-212.
Guinness World Records. (2016). Oldest person (ever). Retrieved from http://www.guinnessworldrecords.com/search?term=oldest+person+%28ever%29
Ha, J. H. (2010). The effects of positive and negative support from children on widowed older adults’ psychological adjustment: A longitudinal analysis. Gerontologist, 50, 471-481.
Harkins, S. W., Price, D. D. & Martinelli, M. (1986). Effects of age on pain perception. Journal of Gerontology, 41, 58-63.
Harvard School of Public Health. (2016). Antioxidants: Beyond the hype. Retrieved from https://www.hsph.harvard.edu/nutritionsource/antioxidants
Hasher, L. & Zacks, R. T. (1988). Working memory, comprehension, and aging: A review and a new view. In G.H. Bower (Ed.), The Psychology of Learning and Motivation, (Vol. 22, pp. 193–225). San Diego, CA: Academic Press.
He, W., Goodkind, D., & Kowal, P. (2016). An aging world: 2015. International Population Reports. U.S. Census Bureau.
He, W., Sengupta, M., Velkoff, V., & DeBarros, K. (2005.). U. S. Census Bureau, Current Popluation Reports, P23-209, 65+ in the United States: 2005 (United States, U. S. Census Bureau). Retrieved from http://www.census.gov/prod/1/pop/p23- 190/p23-190.html
Hendricks, J., & Cutler, S. J. (2004). Volunteerism and socioemotional selectivity in later life. Journal of Gerontology, 59B, S251-S257.
Henry, J. D., MacLeod, M. S., Phillips, L. H., & Crawford, J. R. (2004). A meta-analytic review of prospective memory and aging. Psychology and Aging, 19, 27–39.
Heron, M. (2018). Deaths: Leading causes 2016. National Vital Statistics Reports, 67(6), 1-77.
Hillman, J., & Hinrichsen, G. A. (2014). Promoting and affirming competent practice with older lesbian and gay adults. Professional Psychology: Research and Practice, 45(4), 169-277.
Hinze, S. W., Lin, J., & Andersson, T. E. (2012). Can we capture the intersections? Older black women, education, and health. Women’s Health Issues, 22, e91-e98.
Hirokawa K., Utsuyama M., Hayashi, Y., Kitagawa, M., Makinodan, T., & Fulop, T. (2013). Slower immune system aging in women versus men in the Japanese population. Immunity & Ageing, 10(1), 19.
Holland, K. (2014). Why America’s campuses are going gray? Retrieved from http://www.cnbc.com/2014/08/28/why-americas- campuses-are-going-gray.html
Holmes, T. H., & Rahe, R. H. (1967). The social readjustment rating scale. Journal of psychosomatic research, 11, 213.
Holth, J., Fritschi, S., Wang, C., Pedersen, N., Cirrito, J., Mahan, T.,…Holtzman, D. 2019). The sleep-wake cycle regulates brain interstitial fluid tau in mice and CSF tau in humans. Science, 363(6429), 880-884.
Hooyman, N. R., & Kiyak, H. A. (2011). Social gerontology: A multidisciplinary perspective (9th Ed.). Boston, MA: Pearson James, J. B., Matz-Costa, C., & Smyer, M. A. (2016). Retirement security: It’s not just about the money. American Psychologist, 71(4), 334-344.
Jarrett, C. (2015). Great myths of the brain. West Sussex, UK: John Wiley & Sons.
Jefferies, L. N., Roggeveen, A. B., Ennis, J. T., Bennett, P. J., Sekuler, A. B., & Dilollo, V. (2015). On the time course of attentional focusing in older adults. Psychological Research, 79, 28-41.
Jensen, M. P., Moore, M. R., Bockow, T. B., Ehde, D. M., & Engel, J. M. (2011). Psychosocial factors and adjustment to persistent pain in persons with physical disabilities: A systematic review. Archives of Physical Medicine & Rehabilitation, 92, 146–160. doi:10.1016/j.apmr.2010 .09.021
Jin, K. (2010). Modern biological theories of aging. Aging and Disease, 1, 72-74.
Kahana, E., Bhatta, T., Lovegreen, L. D., Kahana, B., & Midlarsky, E. (2013). Altruism, helping, and volunteering: Pathways to well-being in late life. Journal of Aging and Health, 25(1), 159-187.
Kahn, R. L., & Antonucci, T. C. (1980). Convoys over the life course: Attachment, roles, and social support. In P. B. Baltes & O. G. Brim (Eds.), Life-span development and behavior (pp. 253–286). New York: Academic Press.
Kane, M. (2008). How are sexual behaviors of older women and older men perceived by human service students? Journal of Social Work Education, 27(7), 723-743.
Karraker, A., DeLamater, J., & Schwartz, C. R. (2011). Sexual frequency decline from midlife to later life. The Journal of Gerontology, Series B: Psychological Sciences and Social Sciences, 66B, 502-512.
Kaskie, B., Imhof, S., Cavanaugh, J., & Culp, K. (2008). Civic engagement as a retirement role for aging Americans. The Gerontologist, 48, 368-377.
Kemp, E. A., & Kemp, J. E. (2002). Older couples: New romances: Finding and keeping love in later life. Berkeley, CA: Celestial Arts.
King, V., & Scott, M. E. (2005). A comparison of cohabitating relationships among older and younger adults. Journal of Marriage and Family, 67(2), 271-285.
Kolb, B., & Whishaw, I. Q. (2011). An introduction to brain and behavior (3rd ed.). New York, NY: Worth Publishers.
Kosberg, J. I. (2014). Reconsidering assumptions regarding men an elder abuse perpetrators and as elder abuse victims. Journal of Elder Abuse and Neglect, 26, 207-222.
Kowalski, S. D., & Bondmass, M. D. (2008). Physiological and psychological symptoms of grief in widows. Research in Nursing and Health, 31(1), 23-30.
Kramer, A. F. & Erickson, K. I. (2007). Capitalizing on cortical plasticity: The influence of physical activity on cognition and brain function. Trends in Cognitive Sciences, 11, 342–348.
Lang, F. R., & Schütze, Y. (2002). Adult children’s supportive behaviors and older adults’ subjective well-being: A developmental perspective on intergenerational relationships. Journal of Social Issues, 58, 661-680.
Laslett, P. (1989). A fresh map of life: The emergence of the third age. London, UK: Weidenfeld & Nicolson.
Lee, S.B., Oh, J.G., Park, J.H., Choi, S.P., & Wee, J.H. (2018). Differences in youngest-old, middle-old, and oldest-old patients who visit the emergency department. Clinical and Experimental Emergency Medicine, 5(4), 249-255.
Lee, S. J., Steinman, M., & Tan, E. J. (2011). Volunteering, driving status, and mortality in U.S. retirees. Journal of the American Geriatric Society, 59 (2), 274-280. doi: 10.1111/j.1532-5415.2010.03265x
Lemon, F. R., Bengston, V. L., & Peterson, J. A. (1972). An exploration of activity theory of aging: Activity types and life satisfaction among in-movers to a retirement community. Journal of Geronotology, 27, 511-523.
Levant, S., Chari, K., & DeFrances, C. J. (2015). Hospitalizations for people aged 85 and older in the United States 2000-2010. Centers for Disease Control. Retrieved from http://www.cdc.gov/nchs/data/databriefs/db182.pdf
Levy, B. (2009). Stereotype embodiment: A psychosocial approach to aging. Current Directions in Psychological Science, 18, 332-336.
Lichtenberg, P. A. (2016). Financial exploitation, financial capacity, and Alzheimer’s disease. American Psychologist, 71(4), 312-320.
Lin, I. F. (2008). Consequences of parental divorce for adult children’s support of their frail parents. Journal of Marriage and Family, 70(1), 113-128.
Livingston, G. (2019). Americans 60 and older are spending more time in front of their screens than a decade ago. Retrieved from: https://www.pewresearch.org/fact-tank/2019/06/18/americans-60-and-older-are-spending-more-time-in-front-of- their-screens-than-a-decade-ago/
Luo, L., & Craik, F. I. M. (2008). Aging and memory: A cognitive approach. Canadian Journal of Psychology, 53, 346-353. Martin, L. J. (2014). Age changes in the senses. MedlinePlus. Retrieved from https://medlineplus.gov/ency/article/004013.htm
Martin, P., Poon, L.W., & Hagberg, B. (2011). Behavioral factors of longevity. Journal of Aging Research, 2011/2012, 1–207.
Mayer, J. (2016). MyPlate for older adults. Nutrition Resource Center on Nutrition and Aging and the U. S. Department of Agriculture Human Nutrition Research Center on Aging and Tufts University. Retrieved from http://nutritionandaging.org/my-plate-for-older-adults/
McCormak A., Edmondson-Jones M., Somerset S., & Hall D. (2016) A systematic review of the reporting of tinnitus prevalence and severity. Hearing Research, 337, 70-79.
McCrae, R. R., & Costa, P. T. (1988). Physiological resilience among widowed men and women: A 10 year follow-up study of a national sample. Journal of Social Issues, 44(3), 129-142.
McDonald, L., & Robb, A. L. (2004). The economic legacy of divorce and separation for women in old age. Canadian Journal on Aging, 23, 83-97.
McEntarfer, E. (2018). Older people working longer, earning more. Retrieved from http://thepinetree.net/new/?p=58015
Meegan, S. P., & Berg, C. A. (2002). Contexts, functions, forms, and processes of collaborative everyday problem solving in older adulthood. International Journal of Behavioral Development, 26(1), 6-15. doi: 10.1080/01650250143000283
Molton, I. R., & Terrill, A. L. (2014). Overview of persistent pain in older adults. American Psychologist, 69(2), 197-207. Natanson, H. (2019, July 14). To reduce risk of Alzheimer’s play chess and ditch red meat. The Chicago Tribune, p. 1.
National Council on Aging. (2019). Healthy aging facts. Retrieved from https://www.ncoa.org/news/resources-for-reporters/get- the-facts/healthy-aging-facts/
National Council on Alcoholism and Drug. (2015). Alcohol, drug dependence and seniors. Retrieved from https://www.ncadd.org/about-addiction/seniors/alcohol-drug-dependence-and-seniors
National Eye Institute. (2016a). Cataract. Retrieved from https://nei.nih.gov/health/cataract/
National Eye Institute. (2016b). Glaucoma. Retrieved from https://nei.nih.gov/glaucoma/
National Gay and Lesbian Task Force. (2006). Make room for all: Diversity, cultural competency and discrimination in an aging America. Washington, DC: The Policy Institute of the National Gay and Lesbian Task Force.
National Institutes of Health. (2011). What is alpha-1 antitrypsin (AAT) deficiency? Retrieved from http://www.nhlbi.nih.gov/health/health-topics/topics/aat
National Institutes of Health. (2013). Hypothyroidism. Retrieved from https://www.niddk.nih.gov/health-information/health- topics/endocrine/hypothyroidism/Pages/fact-sheet.aspx
National Institutes of Health. (2014a). Aging changes in hormone production. Retrieved from https://medlineplus.gov/ency/article/004000.htm
National Institutes of Health. (2014b). Cataracts. Retrieved from https://medlineplus.gov/cataract.html
National Institutes of Health. (2014c). Prescription and illicit drug abuse. NIH Senior Health: Built with you in mind. Retrieved from http://nihseniorhealth.gov/drugabuse/illicitdrugabuse/01.html
National Institutes of Health. (2015a). Macular degeneration. Retrieved from https://medlineplus.gov/maculardegeneration.html
National Institutes of Health. (2015b). Pain: You can get help. Retrieved from https://www.nia.nih.gov/health/publication/pain
National Institutes of Health. (2016). Quick statistics about hearing. Retrieved from https://www.nidcd.nih.gov/health/statistics/quick-statistics-hearing
National Institutes of Health: Arthritis and Musculoskeletal and Skin Diseases. (2014). Arthritis and rheumatic diseases. Retrieved from https://www.niams.nih.gov/Health_Info/Arthritis/arthritis_rheumatic.asp
National Institutes of Health: Senior Health. (2013). What is COPD? Retrieved from http://nihseniorhealth.gov/copd/whatiscopd/01.html
National Institutes of Health: Senior Health. (2015). What is osteoporosis? http://nihseniorhealth.gov/osteoporosis/whatisosteoporosis/01.html
National Institutes of Health: Senior Health (2016a). Problems with smell. Retrieved from https://nihseniorhealth.gov/problemswithsmell/aboutproblemswithsmell/01.html
National Institutes of Health: Senior Health (2016b). Problems with taste. Retrieved from https://nihseniorhealth.gov/problemswithtaste/aboutproblemswithtaste/01.html
National Institute on Aging. (2011a). Biology of aging: Research today for a healthier tomorrow. Retrieved from https://www.nia.nih.gov/health/publication/biology-aging/preface
National Institute on Aging. (2011b). Baltimore Longitudinal Study of Aging Home Page. (2011). Retrieved from http://www.grc.nia.nih.gov/branches/blsa/blsa.htm
National Institute on Aging. (2012). Heart Health. Retrieved from https://www.nia.nih.gov/health/publication/heart-health
National Institute on Aging. (2013). Sexuality later in life. Retrieved from https://www.nia.nih.gov/health/publication/sexuality- later-life
National Institute on Aging. (2015a). The Basics of Lewy Body Dementia. Retrieved from https://www.nia.nih.gov/alzheimers/publication/lewy-body-dementia/basics-lewy-body-dementia
National Institute on Aging. (2015b). Global Health and Aging. Retrieved from https://www.nia.nih.gov/research/publication/global-health-and-aging/living-longer
National Institute on Aging. (2015c). Hearing loss. Retrieved from https://www.nia.nih.gov/health/publication/hearing-loss
National Institute on Aging. (2015d). Humanity’s aging. Retrieved from https://www.nia.nih.gov/research/publication/global- health-and-aging/humanitys-aging
National Institute on Aging. (2015e). Shingles. Retrieved from https://www.nia.nih.gov/health/publication/shingles
National Institute on Aging. (2015f). Skin care and aging. Retrieved from https://www.nia.nih.gov/health/publication/skin-care- and-aging
National Institute on Aging. (2016). A good night’s sleep. Retrieved from https://www.nia.nih.gov/health/publication/good- nights-sleep
National Library of Medicine. (2014). Aging changes in body shape. Retrieved from https://medlineplus.gov/ency/article/003998.htm
National Library of Medicine. (2019). Aging changes in the heart and blood vessels. Retrieved from https://medlineplus.gov/ency/article/004006.htm
National Osteoporosis Foundation. (2016). Preventing fractures. Retrieved from https://www.nof.org/prevention/preventing- fractures/
National Sleep Foundation. (2009). Aging and sleep. Retrieved from https://sleepfoundation.org/sleep-topics/aging- and-sleep
Nelson, T. D. (2016). Promoting healthy aging by confronting ageism. American Psychologist, 71(4), 276-282.
Novotney, A. (2019). Social isolation: It could kill you. Monitor on Psychology, 50(5), 33-37.
Office on Women’s Health. (2010a). Raising children again. Retrieved from http://www.womenshealth.gov/aging/caregiving/raising-children-again.html
Office on Women’s Health. (2010b). Sexual health. Retrieved from http://www.womenshealth.gov/aging/sexual-health/
Olanow, C. W., & Tatton, W. G. (1999). Etiology and pathogenesis of Parkinson’s disease. Annual Review of Neuroscience, 22, 123-144.
Ortman, J. M., Velkoff, V. A., & Hogan, H. (2014). An aging nation: The older population in the United States. United States Census. Retrieved from http://www.census.gov/prod/2014pubs/p25-1140.pdf
Overstreet, L. (2006). Unhappy birthday: Stereotypes in late adulthood. Unpublished manuscript, Texas Woman’s University.
Owsley, C., Rhodes, L. A., McGwin Jr., G., Mennemeyer, S. T., Bregantini, M., Patel, N., … Girkin, C. A. (2015). Eye care quality and accessibility improvement in the community (EQUALITY) for adults at risk for glaucoma: Study rationale and design. International Journal for Equity in Health, 14, 1-14. DOI 10:1186/s12939-015-0213-8
Papernow, P. L. (2018). Recoupling in midlife and beyond: From love at last to not so fast. Family Processes, 57(1), 52-69. Park, D. C. & Gutchess, A. H. (2000). Cognitive aging and everyday life. In D.C. Park & N. Schwarz (Eds.), Cognitive Aging: A Primer (pp. 217–232). New York: Psychology Press.
Park, D. C., & Reuter-Lorenz, P. (2009). The adaptive brain: Aging and neurocognitive scaffolding. Annual Review of Psychology, 60, 173-196.
Pew Research Center. (2011). Fighting poverty in a tough economy. Americans move in with their relatives. Retrieved from http://www.pewsocialtrends.org/files.2011/10.Multigenerationsl-Households-Final1.pdf
Pilkington, P. D., Windsor, T. D., & Crisp, D. A. (2012). Volunteerism and subjective well-being in midlife and older adults: The role of supportive social networks. Journal of Gerontology Series B: Psychological and Social Sciences, 67 B (2), 249- 260. Doi:10.1093/geronb/grb154.
Quinn, J. F., & Cahill, K. E. (2016). The new world of retirement income security in America. American Psychologist, 71(4), 321-333.
Resnikov, S., Pascolini, D., Mariotti, S. P., & Pokharel, G. P. (2004). Global data on visual impairment in the year 2002. Bulletin of the World Health Organization, 82, 844-851.
Rhodes, M. G., Castel, A. D., & Jacoby, L. L. (2008). Associative recognition of face pairs by younger and older adults: The role of familiarity-based processing. Psychology and Aging, 23, 239-249.
Riediger, M., Freund, A.M., & Baltes, P.B. (2005). Managing life through personal goals: Intergoal facilitation and intensity of goal pursuit in younger and older adulthood. Journals of Gerontology, 60B, P84-P91.
Roberto, K. A. (2016). The complexities of elder abuse. American Psychologist, 71(4), 302-311.
Robin, R. C. (2010). Grown-up, but still irresponsible. New York Times. Retrieved from http://www.nytimes.com/2010/10/10weekinreview/10rabin.html>.
Robins, R.W., & Trzesniewski, K.H. (2005). Self-esteem development across the lifespan. Current Directions in Psychological Science, 14 (3), 158-162. DOI: 10.1111/j.0963- 7214.2005.00353x
Rowe, J. W. & Kahn, R. L. (1997). Successful aging. The Gerontologist, 37(4), 433–440.
Rubinstein, R.L. (2002). The third age. In R.S. Weiss & S.A. Bass (Eds.), Challenges of the third age; Meaning and purpose in later life (pp. 29-40). New York: Oxford University Press.
Ruckenhauser, G., Yazdani, F., & Ravaglia, G. (2007). Suicide in old age: Illness or autonomous decision of the will? Archives of Gerontology and Geriatrics, 44(6), S355-S358.
Saiidi, U. (2019). US life expectancy has been declining. Here’s why. Retrieved from https://www.cnbc.com/2019/07/09/us-life- expectancy-has-been-declining-heres-why.html
Salthouse, T. A. (1984). Effects of age and skill in typing. Journal of Experimental Psychology: General, 113, 345.
Salthouse, T. A. (1996). The processing-speed theory of adult age differences in cognition. Psychological Review, 103, 403-428. Salthouse, T. A. (2004). What and when of cognitive aging. Current Directions in Psychological Science, 13(4), 140-144.
Salthouse, T. A., & Babcock, R. L. (1991). Decomposing adult age differences in working memory. Developmental Psychology, 27, 763-776.
Schacter, D. L., Church, B. A., & Osowiecki, D. O. (1994). Auditory priming in elderly adults: Impairment of voice-specific implicit memory. Memory, 2, 295-323.
Schaie, K. W. (1994). The course of adult intellectual development. American Psychologist, 49, 304-311.
Schick, V., Herbenick, D., Reece, M., Sanders, S. A., Dodge, B., Middlestadt, S. E., & Fortenberry, J. D. (2010). Sexual behaviors, condom use, and sexual health of Americans over 50: Implications for sexual health promotion for older adults. Journal of Sexual Medicine, 7(5), 315-329.
Schwartz, B. L. (2011). Memory: Foundations and applications. Thousand Oaks, CA: Sage Publications. Scott, P. J. (2015). Save the Males. Men’s Health. Retrieved from http://www.menshealth.com
Shmerling, R. H. (2016). Why men often die earlier than women. Harvard Health Publications. Retrieved from http://www.health.harvard.edu/blog/why-men-often-die-earlier-than-women-201602199137
Shokri-Kojori, E., Wang, G., Wiers, C., Demiral, S., Guo, M., Kim, S.,…Volkow, N. (2018). β-amyloid accumulation in the human brain after one night of sleep deprivation. Proceedings of the National Academy of Sciences of the United States of America, 115(17), 4483-4488.
Singer, T., Verhaeghen, P., Ghisletta, P., Lindenberger, U., & Baltes, P.B. (2003). The fate of cognition in very old age: Six-year longitudinal findings in the Berlin Aging Study (BASE). Psychology and Aging, 18, 318-331.
Siriwardena, A. N., Qureshi, A., Gibson, S., Collier, S., & Lathamn, M. (2006). GP’s attitudes to benzodiazepine and “z-drug” prescribing: A barrier to implementation of evidence and guidance on hypnotics. British Journal of General Practice, 56, 964-967.
Smith, J. (2000). The fourth age: A period of psychological mortality? Max Planck Forum, 4, 75-88.
Social Security Administration. (2016). Retirement planner: Benefits by year of birth. Retrieved from https://www.ssa.gov/planners/retire/agereduction.html
Sohn, H. (2015). Health insurance and divorce: Does having your own insurance matter? Journal of Marriage and Family, 77, 982-995.
Spaniol, J., Madden, D. J., & Voss, A. (2006). A diffusion model analysis of adult age differences in episodic and semantic long- term memory retrieval. Journal of Experimental Psychology, 32(1). 101-117.
Staudinger, U. M., & Gluck, J. (2011). Psychological wisdom research: Commonalities and differences in a growing field. Annual Review of Psychology, 62, 215–241.
Stepler, R. (2016a). Gender gap in share of older adults living alone narrows. Pew Research Center. Retrieved from http://www.pewsocialtrends.org/2016/02/18/1-gender-gap-in-share-of-older-adults-living-alone-narrows/
Stepler, R. (2016b). Living arrangements of older adults by gender. Pew Research Center Retrieved from http://www.pewsocialtrends.org/2016/02/18/2-living-arrangements-of-older-americans-by-gender/
Stepler, R. (2016c). Smaller share of women 65 or older are living alone. Pew Research Center. Retrieved from http://www.pewsocialtrends.org/2016/02/18/smaller-share-of-women-ages-65-and-older-are-living-alone/
Stepler, R. (2016d). Well-being of older adults living alone. Pew Research Center. Retrieved from http://www.pewsocialtrends.org/2016/02/18/3-well-being-of-older-adults-living-alone/
Stepler, R. (2016e). World’s centenarian population projected to grow eightfold by 2050. Pew Research Center. Retrieved from http://www.pewresearch.org/fact-tank/2016/04/21/worlds-centenarian-population-projected-to-grow-eightfold-by- 2050/
Stoller, E. P., & Longino, C. F. (2001). “Going home” or “leaving home”? The impact of person and place ties on anticipated counterstream migration. Gerontologist, 41, 96-102.
Strait, J.B., & Lakatta, E.G. (2012). Aging-associated cardiovascular changes and their relationship to heart failure. Heart Failure Clinics, 8(1), 143-164.
Strine, T. W., Hootman, J. M., Chapman, D. P., Okoro, C. A., & Balluz, L. (2005). Health-related quality of life, health risk behaviors, and disability among adults with pain-related activity difficulty. American Journal of Public Health, 95, 2042–2048. doi:10.2105/AJPH.2005 .066225
Strough, J., Hicks, P. J., Swenson, L. M., Cheng, S., & Barnes, K. A. (2003). Collaborative everyday problem solving: Interpersonal relationships and problem dimensions. International Journal of Aging and Human Development, 56, 43- 66.
Subramanian, S. V., Elwert, F., & Christakis, N. (2008). Widowhood and mortality among the elderly: The modifying role of neighborhood concentration of widowed individuals. Social Science and Medicine, 66, 873-884.
Sullivan, A. R., & Fenelon, A. (2014). Patterns of widowhood mortality. Journal of Gerontology Series B: Psychological and Social Sciences, 69B, 53-62.
Tales, A., Muir, J. L., Bayer, A., & Snowden, R. J. (2002). Spatial shifts in visual attention in normal aging and dementia of the Alzheimer type. Neuropsychologia, 40, 2000-2012.
Taylor, R., Chatters, L. & Leving, J. (2004). Religion in the lives of African Americans. Thousand Oaks, CA: Sage
Tennstedt, S., Morris, J., Unverzagt, F., Rebok, G., Willis, S., Ball, K., & Marsiske, M. (2006). ACTIVE: Advanced Cognitive Training for Independent and Vital Elderly Clinical Trial. Clinical Trials Database and Worldwide Listings. Retrieved from http://www.clinicaltrialssearch.org/active-advanced-cognitive-training-for-independent-and-vital-elderly- nct00298558.html
Tentori, K., Osherson, D., Hasher, L., & May, C. (2001). Wisdom and aging: Irrational preferences in college students but not older adults. Cognition, 81, B87–B96.
Thornbury, J. M., & Mistretta, C. M. (1981). Tactile sensitivity as a function of age. Journal of Gerontology, 36(1), 34-39.
Tobin, M., K., Musaraca, K., Disouky, A., Shetti, A., Bheri, A. Honer, W. G.,…Lazarov, O. (2019). Human hippocampal neurogenesis persists in aged adults and Alzheimer’s disease patients. Cell Stem Cell, 24(6), 974-982.
Tsang, A., Von Korff, M., Lee, S., Alonso, J., Karam, E., Angermeyer, M. C., . . . Watanabe, M. (2008). Common persistent pain conditions in developed and developing countries: Gender and age differences and comorbidity with depression- anxiety disorders. The Journal of Pain, 9, 883–891. doi:10.1016/j.jpain.2008.05.005
United States Census Bureau. (2012). 2012 national population projections. Washington, DC: Author. Retrieved from https://www.census.gov/population/projections/data/natiobnal/2012.html
United States Census Bureau. (2014a). American Community Survey, 2014 Estimates: table B10001. Retrieved from at http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_14_5YR_B10001&prodType=t able
United States Census Bureau. (2014b). U. S. population projections: 2014-2060. Retrieved from https://www.census.gov/population/projections/data/natiobnal/2014.html
United States Department of Health and Human Services. (2012). A profile of older Americans: 2012. Retrieved from http://www.aoa.gov/Aging_Statistics/Profile/2012/docs/2012profile.pdf
United States Government Accountability Office. (2011). Income security: Older adults and the 2007-2009 recession.
Washington, DC: Author. United States, National Center for Health Statistics. (2002). National Vital Statistics Report, 50(16). Retrieved May 7, 2011, from http://www.cdc.gov/nchs/data/dvs/LCWK1_2000.pdf
United States National Library of Medicine. (2019). Aging changes in hair and nails. Retrieved from https://medlineplus.gov/ency/article/004005.htm
United States Senate Commission on Long-Term Care. (2013). Report to the Congress. Washington, DC: U. S. Government Printing Office.
Vespa, J. & Schondelmyer, E. (2014). A gray revolution in living arrangements. Retrieved from http://blogs.census.gov/2015/07/14/a-gray-revolution-in-living-arrangements/
Viña, J., Borrás, C., Gambini, J., Sastre, J., Pallardó, F.V. (2005). Why females live longer than males: Control of longevity by sex hormones. Science of Aging Knowledge Environment, 23, 17.
Washington University School of Medicine. (2019). Alzheimer’s missing link ID’d, answering what tips brain’s decline. Retrieved from https://medicalxpress.com/news/2019-06-alzheimer-link-idd-brain-decline.html
Wasscher, E., Schneider, D., Hoffman, S., Beste, C., & Sänger, J. (2012). When compensation fails: Attentional deficits in healthy ageing caused by visual distraction. Neuropsychologia, 50, 3185-31-92.
Watson, W. K., & Stelle, C. (2011). Dating for older women: Experiences and meanings of dating in later life. Journal of Women and Aging, 23, 263-275.
Webmd. (2016). Sarcopenia with aging. Retrieved from http://www.webmd.com/healthy- aging/sarcopenia-with-aging
Wilcox, B. J. Wilcox, D. C., & Ferrucci, L. (2008). Secrets of healthy aging and longevity from exceptional survivors around the globe: Lessons from octogenarians to supercentenarians. Journal of Gerontology, 63(11), 1181-1185.
Williamson, E. M., & Evans, F. J. (2000). Cannabinoids in clinical practice. Drugs, 60, 1303-1314. World Health Organization. (2019). World health statistics 2019. Retrieved from: https://apps.who.int/iris/bitstream/handle/10665/324835/9789241565707-eng.pdf
Wright, K. B., & Query, J. L. (2004). Online support and older adults: A theoretical examination of benefits and limitations of computer-mediated support networks for older adults and possible health outcomes. In J. Nussbaum & J. Coupland (Eds.), Handbook of communication and aging research (2nd ed., pp. 499–519). Mahwah, NJ: Erlbaum.
Wrzus, C., Hanel, M., Wagner, J., & Neyer, F. J. (2013). Social network changes and life events across the lifespan: A meta- analysis. Psychological Bulletin, 139(1), 53-80.
Wu, C., Odden, M. C., Fisher, G. G., & Stawski, R. S. (2016). Association of retirement age with mortality: a population-based longitudinal study among older adults in the USA. Journal of Epidemiology and Community Health. doi:10.1136/jech- 2015-207097
Wu, Z., & Schimmele, C. M. (2007). Uncoupling in late life. Generations, 31(3), 41-46.
Xu, J., Murphy, S. L., Kochanek, K. D., & Bastian, B. A. (2016). Deaths: Final data for 2013. National Vital Statistics Report, 64(2), 1-119.
Youdin, R. (2016). Psychology of Aging 101. New York: Springer Publishing.
Zahodne, L. B., Stern, Y., & Manly, J. (2015). Differing effects of education on cognitive decline in diverse elders with low versus high educational attainment. Neuropsychology, 29(4), 649-657.
Attribution
Adapted from Chapter 9 from Lifespan Development: A Psychological Perspective Second Edition by Martha Lally and Suzanne Valentine-French under the Creative Commons Attribution-Noncommercial-Share Alike 3.0 unported license.