7 Ventricular Arrhythmias
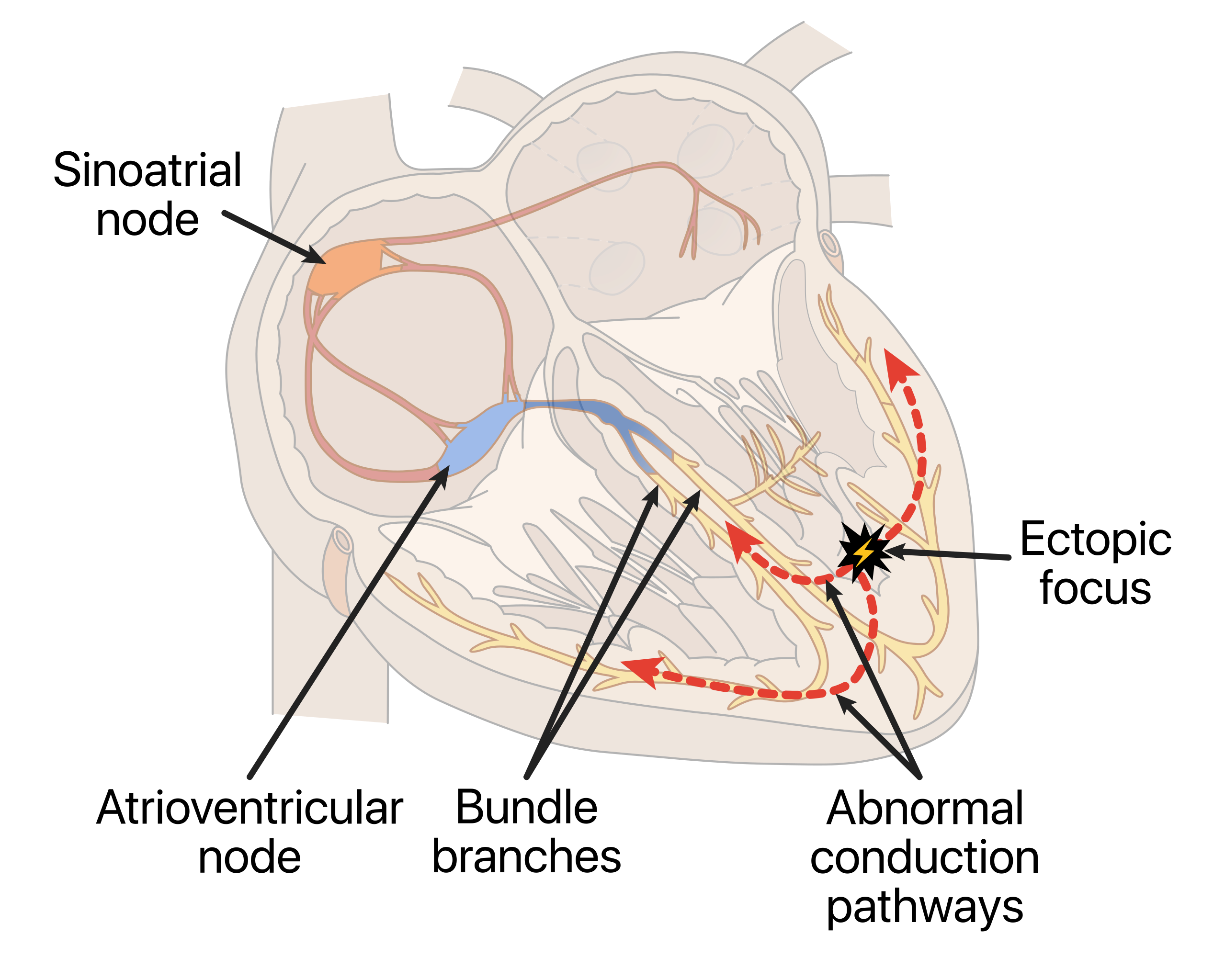
These abnormal heart rhythms originate in the ventricles and can vary from relatively benign premature ventricular contractions (PVCs) to life-threatening ventricular tachycardia (V-tach) and ventricular fibrillation (V-fib). On an EKG, ventricular arrhythmias are characterized by wide QRS complexes (≥0.12 secs), reflecting the abnormal, delayed conduction pathway through the ventricular myocardium rather than the normal conduction system. The T wave and QRS complex deflect in opposite directions on the isoelectric line of the EKG because of differences in action potentials during ventricular depolarization and repolarization. Additionally, the P wave is absent, resulting in the loss of the atrial kick, which can decrease cardiac output by up to 30%. In cases of continuous ventricular arrhythmias, patients may exhibit signs of cardiac decompensation such as hypotension, angina, syncope, and respiratory distress.
1. Premature Ventricular Contractions
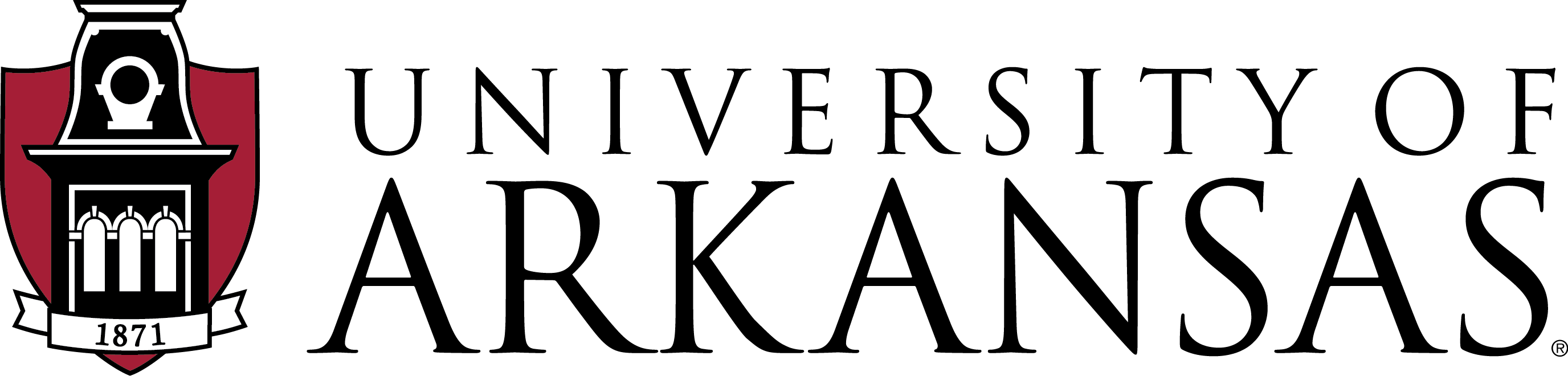
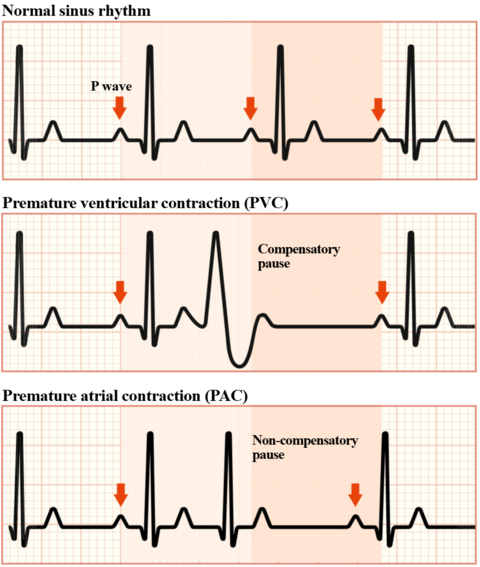
Originating from the ventricles, below the AV node, PVCs are early heartbeats that occur when an ectopic focus within the ventricles initiates a heartbeat before the normal beat from the SA node (see Figure 7.1). These abnormal contractions manifest as palpitations or a “skipped beat” feeling in the chest and are commonly observed in both healthy individuals and those with underlying heart conditions. While often harmless, frequent PVCs may signal an underlying heart condition that warrants evaluation. Again, an isolated PVC is common and often nothing to stress over, but consistently experiencing PVCs could indicate a more serious issue that may require medical attention.
Characteristics of PVCs
- Rhythm: PVCs disrupt the regular heart rhythm, interrupting the regularity of the underlying rhythm
- Rate: Determined from the underlying rhythm
- P wave: PVCs may not have a preceding P wave, as the impulse does not originate from the atria. If present, the P wave may be inverted or retrograde due to the reversed atrial activation sequence
- PR interval: Typically not measurable for PVCs, as the impulse does not follow the normal conduction pathway
- QRS complex: Wide and bizarre, measuring at least 0.12 secs
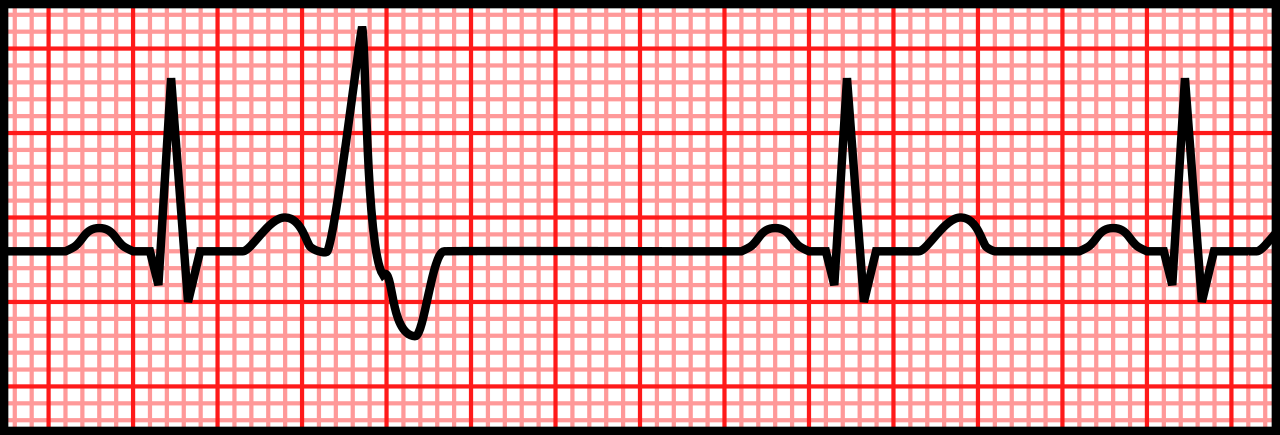
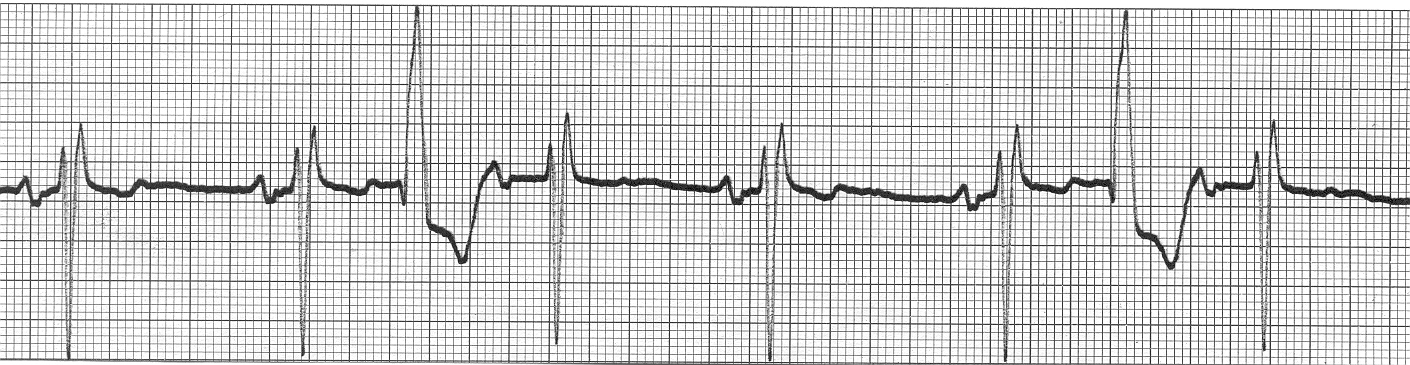
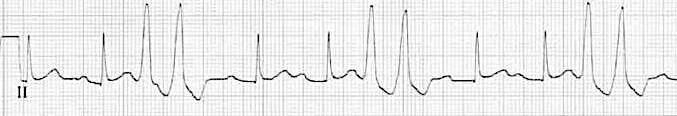
**One characteristic feature often seen after a PVC is a compensatory pause. This compensatory pause in the rhythm refers to the temporary slowing of the rate immediately following a PVC. During this pause, the total time from the PVC to the next regular heartbeat is about the same length of time as two normal heartbeats, as shown below in Figure 7.3. The compensatory pause represents the heart’s compensatory mechanism to maintain proper timing and prevent the ectopic PVC beat from disrupting the underlying sinus rhythm. It allows the next sinus node impulse to resume control of the heart’s pacemaker function after the transient PVC event. This pause helps re-establish the regular rhythm and ensures the premature beat does not continuously pre-excite the heart’s conduction system.
Different Types of PVCs
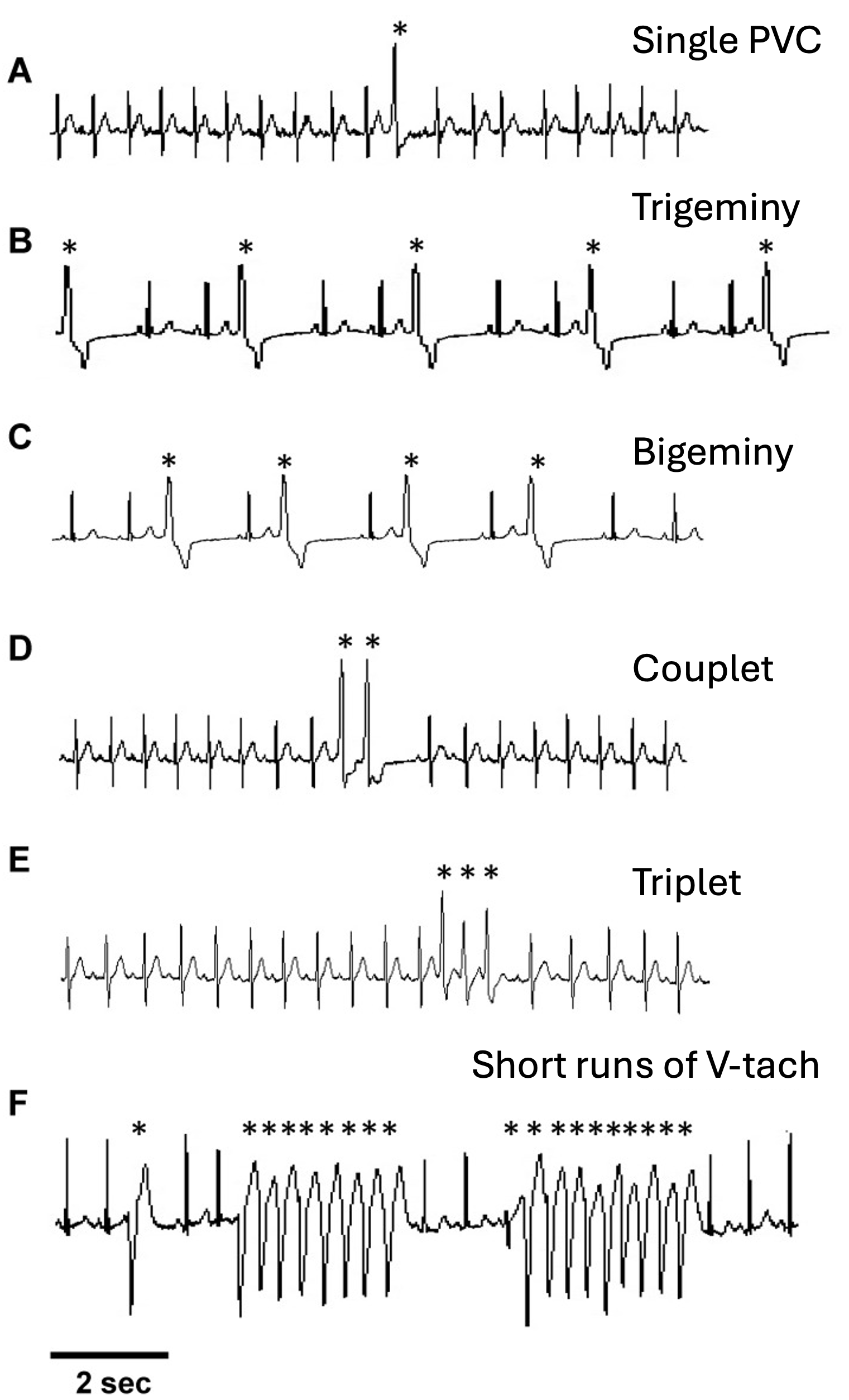
There are several types and combinations of PVCs, and the more variations observed, the more concerning it can be for the patient’s condition. Premature ventricular contractions are classified based on their frequency, morphology, and timing on the EKG. Below are some of the main types of PVCs:
Interpolated PVC
- Unlike typical PVCs, an interpolated PVC occurs between two normal sinus beats without causing a compensatory pause. This phenomenon is more likely to arise when the underlying sinus rate is relatively slow, allowing the ventricles to recover excitability in time for the next scheduled sinus beat.
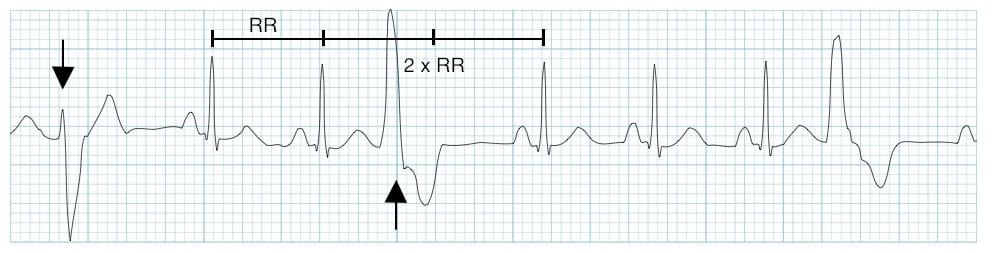
Unifocal PVCs
- These PVCs originate from a single ectopic focus within the ventricles. They exhibit a consistent morphology and timing on the EKG, appearing uniform in shape and size.

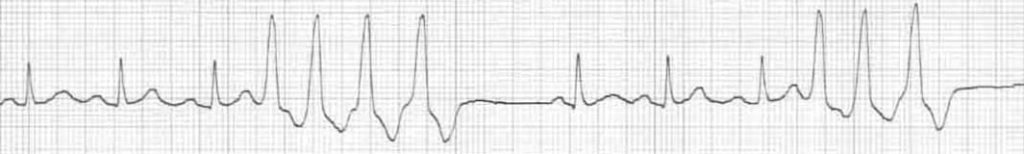
Multifocal PVCs
- These PVCs arise from multiple ectopic foci within the ventricles. They are considered more serious than unifocal PVCs due to their varying morphologies and timings, indicating potential involvement of different regions of the ventricular myocardium.
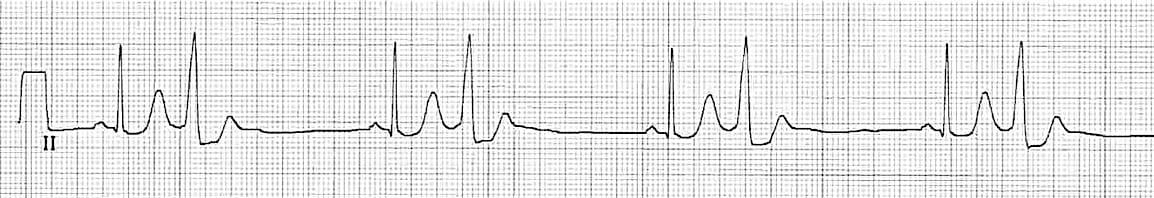
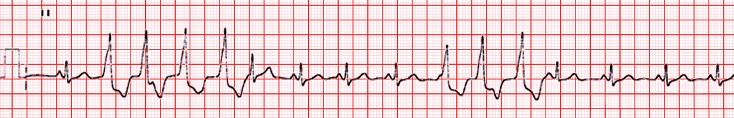
Bigeminal PVCs
- In this pattern, a PVC occurs after every other normal sinus beat, resulting in an alternating pattern of normal beats and PVCs.
Trigeminal PVCs
- Here, a PVC occurs after every two normal sinus beats. This creates a pattern where every third beat is a PVC.

Couplets
- A couplet refers to two consecutive PVCs occurring together on the EKG.
- Three to 30 consecutive PVCs with a rate >100 bpm are classified as non-sustained ventricular tachycardia (NSVT), not individual PVCs.
- If the rate of the consecutive PVCs is <100 bpm, it is referred to as a ventricular rhythm rather than NSVT or individual PVCs.
Run of Ventricular Tachycardia
- A run of V-tach is defined as three or more consecutive PVCs occurring in a row. Also known as a “salvo.”
Sustained Ventricular Tachycardia
- When more than 30 consecutive beats are PVCs with a rate >100 bpm, it is known as sustained ventricular tachycardia.
R-on-T Phenomenon
- This potentially dangerous situation occurs when a PVC falls on the T wave of the preceding beat, during the early repolarization phase of the ventricular myocardium. Since the cells have not fully repolarized, this phenomenon can trigger sustained ventricular tachycardia or ventricular fibrillation.

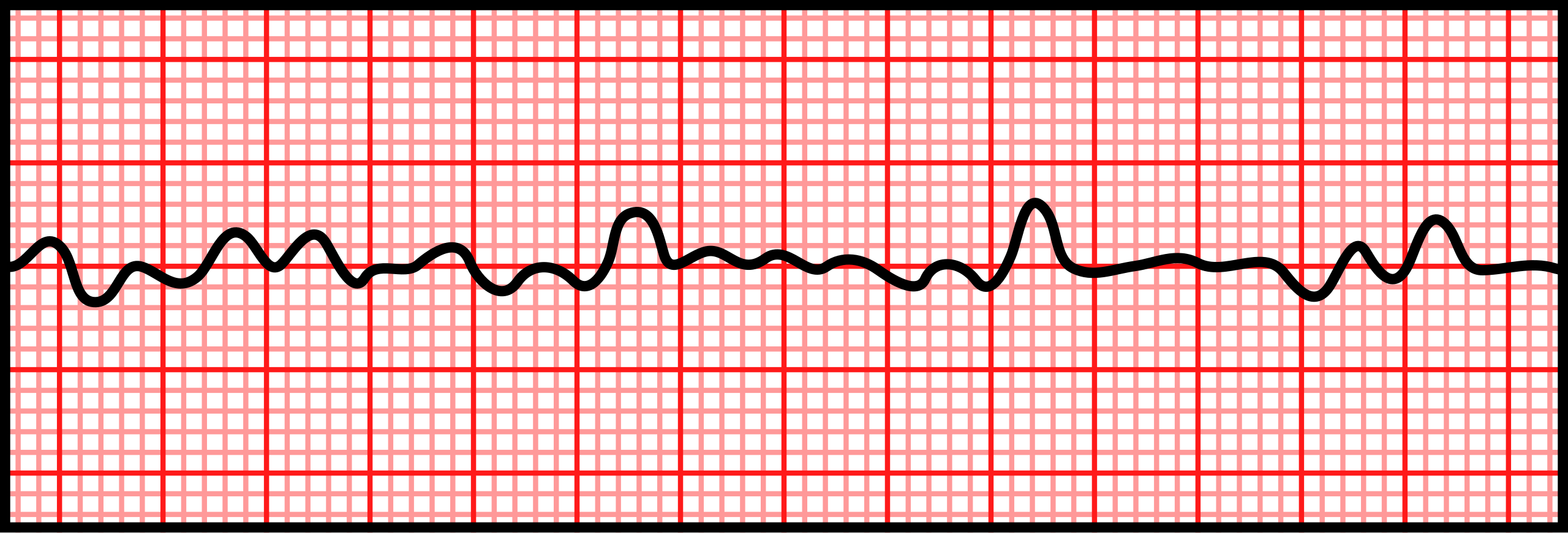
2. Idioventricular Rhythm
Also known as the “rhythm of last resort,” an idioventricular rhythm is a slow, regular heart rhythm that originates from the ventricles when the normal pacemaker of the heart, the SA node, fails to generate impulses or when these impulses are blocked from reaching the ventricles. Thus, the cells of the His-Purkinje network become the driving pacemaker of the heart. This rhythm serves as a “backup” pacemaker, ensuring that the heart continues to beat, albeit at a slower rate than the normal SA node pace. Idioventricular rhythm is characterized by wide QRS complexes and a rate typically between 20–40 bpm.
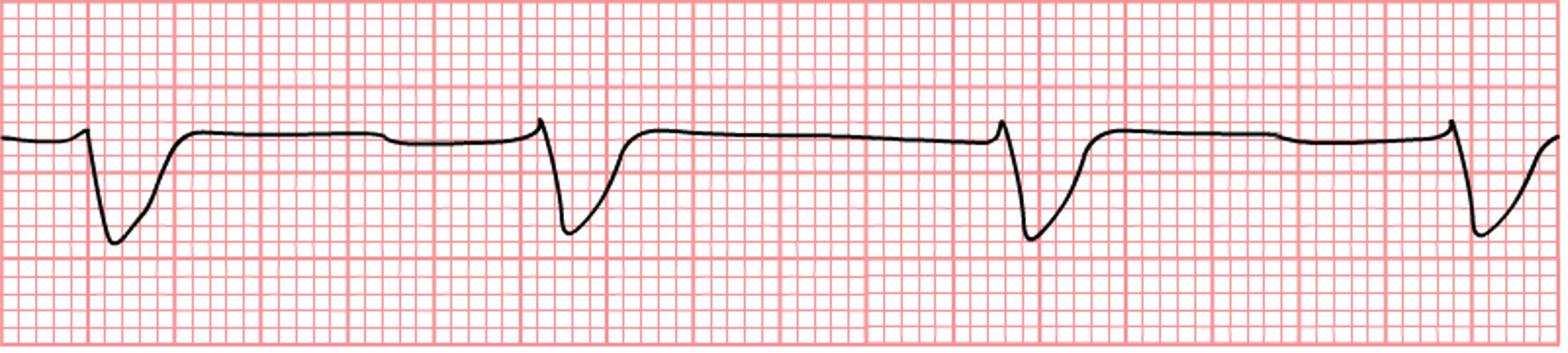
Characteristics of Idioventricular Rhythm
- Rhythm: Usually regular, but may have slight variations in R-R intervals
- Rate: Typically 20–40 bpm, but can become slower than 20 bpm or occasionally reach up to 60 bpm
- P wave: Absent. If present, not related to QRS complexes
- PR interval: Not applicable due to absence of P waves
- QRS complex: Wide and bizarre in appearance, usually >0.12 secs
- Tolerance: Often well-tolerated if rate is adequate to maintain cardiac output for ample perfusion. If rate drops below 20 bpm, or perfusion is poor, signs of cardiac decompensation can present, such as hypotension and decreased consciousness. In severe cases, this may result in cardiac arrest and mortality.
Clinical Significance
- Indicates a failure of higher pacemaker sites (i.e., SA node, AV node) to control the heart rhythm
- May be a sign of underlying heart disease or electrolyte imbalances
- Can be a transitional rhythm in cardiac arrest situations
Signs & Symptoms
- Often asymptomatic if the rate is adequate to maintain cardiac output
- Possible symptoms include fatigue, dizziness, or lightheadedness due to reduced cardiac output
- In some cases, patients may experience palpitations
Treatment
- Often no immediate treatment is required if the patient is hemodynamically stable
- Addressing underling causes (e.g., correcting electrolyte imbalance, treating ischemia)
- In symptomatic cases, atropine or temporary pacing may be considered to increase heart rate
- Long-term management may involve permanent pacemaker implantation if the underlying cause cannot be corrected
Causes
- Acute myocardial infarction
- Digitalis toxicity
- Electrolyte imbalances, particularly hyperkalemia
- Increased vagal tone or conditions causing advanced or complete heart block
3. Accelerated Idioventricular Rhythm
A ventricular rhythm characterized by a faster rate than typical idioventricular rhythm but slower than V-tach. It occurs when the ventricles take over the heart’s pacing, often because higher pacemaker sites (i.e., SA node, AV node) are suppressed or the ventricular pacemaker is more active. Accelerated idioventricular rhythm (AIVR) frequently appears during myocardial ischemia or reperfusion and can act as an intermediary rhythm in different clinical situations. It can occur in short or longer episodes that resolve on their own. The heart returns to normal sinus rhythm (NSR) when the SA node speeds up and regains control as the primary pacemaker of the heart.
Characteristics of AIVR
- Rhythm: Usually regular, but may show slight R-R interval variations
- Rate: Typically between 60–100 bpm
- P wave: Usually absent. If present, not related to QRS complexes
- PR interval: Not applicable due to absence of P waves
- QRS complex: Wide and bizarre in appearance, usually >0.12 secs
- Tolerance: Often well-tolerated due to adequate cardiac output. Patient may be asymptomatic or present mild symptoms
Clinical Significance
- Often a marker of reperfusion after myocardial infarction
- Considered a benign heart rhythm in general
- Can indicate underlying cardiac or metabolic disorders, but can occur without apparent heart diseases
- Usually a transient rhythm that resolves spontaneously
Signs & Symptoms
- Often asymptomatic due to the rate being fast enough to maintain sufficient cardiac output
- Some patients may experience palpitations or mild dizziness
- Rarely causes significant hemodynamic instability
Treatment
- Usually self-limiting and does not require specific treatment
- Address underlying causes (e.g., correct electrolyte imbalance, treat ischemia)
- Avoid antiarrhythmic drugs (e.g., lidocaine) unless the AIVR causes hemodynamic instability
- In rare cases of persistent symptomatic AIVR, atropine or temporary pacing may be considered
Causes
- Reperfusion after acute myocardial infarction
- Digitalis toxicity
- Electrolyte imbalances, especially hypokalemia or hypomagnesemia
- Post-cardiac surgery
- Cardiomyopathies
- Cocaine or other stimulant use
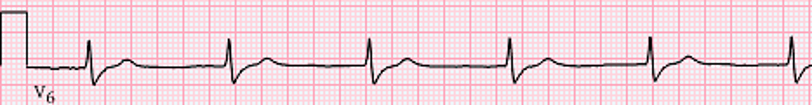
4. Ventricular Tachycardia
A fast, serious rhythm originating from the ventricles that is characterized by a heart rate >100 bpm and can be life-threatening if not promptly treated. Ventricular tachycardia (V-tach) can occur in short bursts, known as non-sustained V-tach, or persist for longer periods, known as sustained V-tach, potentially leading to more severe arrhythmias like ventricular fibrillation.
Characteristics of Ventricular Tachycardia
- Rhythm: Usually regular, but can be slightly irregular in some cases
- Rate: Typically between 100–250 bpm
- P wave: Usually absent or not related to QRS complexes. If present, P waves are often buried within the QRS complexes
- PR interval: Not applicable due to the absence of a consistent relationship between P waves and QRS complexes
- QRS complex: Wide and bizarre in appearance, usually >0.12 secs. Usually difficult to distinguish between QRS and T wave. Uniform (i.e., monomorphic) or varying (i.e., polymorphic) in shape
- Tolerance: Can be poorly tolerated, especially if sustained V-tach. May lead to hypotension, varying heart sounds, congestive heart failure, shock, or ventricular fibrillation. Can lead to hemodynamic instability and cardiac arrest
Clinical Significance
- Indicates serious underlying heart disease, such as ischemic heart disease or cardiomyopathy
- Can lead to life-threatening arrhythmias like ventricular fibrillation
- Requires prompt medical evaluation and treatment
Signs & Symptoms
- Palpitations or a sensation of rapid heartbeats
- Dizziness or lightheadedness
- Chest pain or discomfort
- In severe cases, shortness of breath and syncope
Treatment
- Immediate treatment of sustained V-tach includes antiarrhythmic medications (e.g., amiodarone, lidocaine)
- Electrical cardioversion or defibrillation for unstable patients
- Long-term management may involve implantable cardioverter-defibrillators (ICDs) or catheter ablation
- Addressing underlying causes, such as ischemia or electrolyte imbalances
Causes
- Ischemic heart disease, particularly post-MI
- Cardiomyopathies, including hypertrophic and dilated cardiomyopathy
- Electrolyte imbalances, such as hypokalemia or hyperkalemia
- Drug toxicity, including digitalis or antiarrhythmia drugs
- Structural heart abnormalities or congenital heart disease
- R-on-T phenomenon
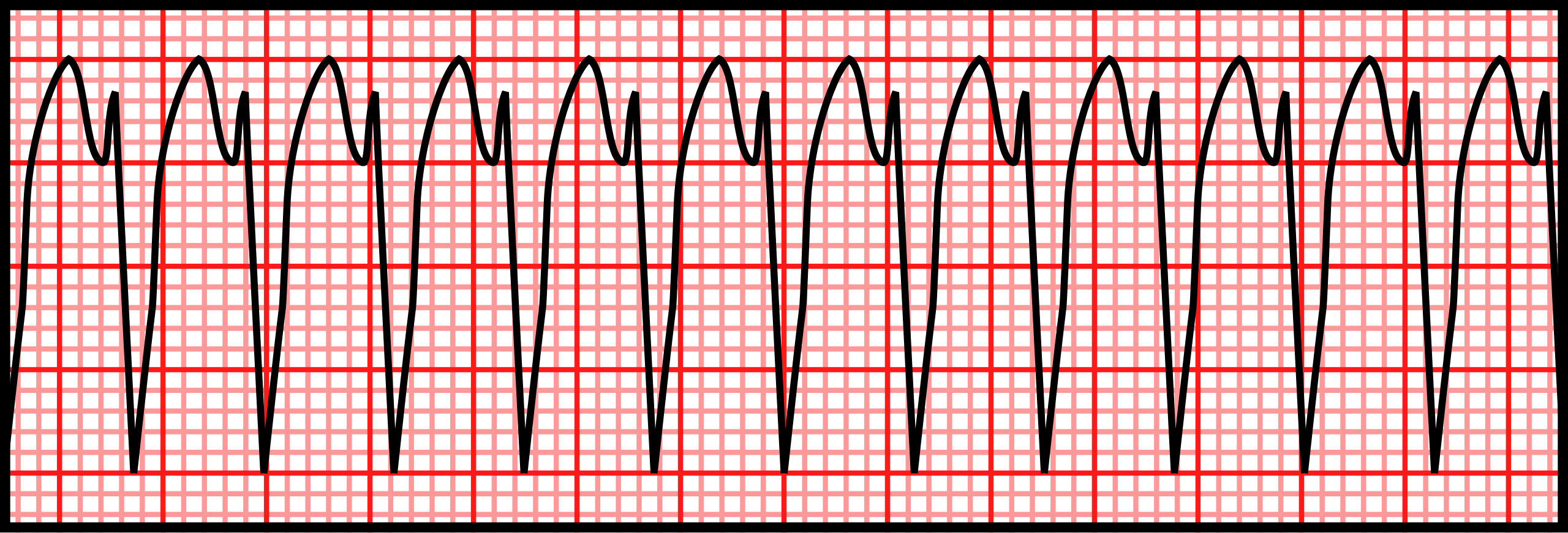
5. Torsades de Pointes
The name “Torsades de Pointes” is French for “twisting of the points.” It is a specific type of polymorphic V-tach characterized by a distinctive “twisting” pattern of the QRS complexes around the isoelectric line on an EKG. Torsades de Pointes is a potentially life-threatening arrhythmia often associated with a prolonged QT interval and can lead to ventricular fibrillation (V-fib) and sudden cardiac death if not promptly addressed.

Characteristics of Torsades de Pointes
- Rhythm: Irregular, but can be regular at times
- Rate: Typically between 150–250 bpm
- P wave: Usually not visible due to the rapid ventricular activity
- PR interval: Not applicable due to absence of visible P waves
- QRS complex: Wide (>0.12 secs) and polymorphic, with a characteristic twisting appearance. Amplitude and morphology change progressively, creating spindle-shaped tracing
- Tolerance: Can be poorly tolerated due to rapid rate and ineffective cardiac output, however, 50% of patients are asymptomatic. Can quickly lead to hemodynamic instability and loss of consciousness
Clinical Significance
- Indicates a critical condition with high risk of progression to V-fib
- Often associated with prolonged QT interval, requiring immediate intervention
- Can be a marker of underlying electrolyte imbalances or drug toxicities
Signs & Symptoms
- Palpitations or sensation of rapid, irregular heartbeats
- Dizziness, lightheadedness, or syncope
- Shortness of breath and chest discomfort
- Sudden cardiac arrest in severe cases
- Around 50% of patients experiencing Torsades de Pointes are asymptomatic
Treatment
- Immediate discontinuation of QT-prolonging medications, if applicable
- Correction of electrolyte imbalances, particularly hypokalemia and hypomagnesemia
- Intravenous magnesium sulfate as first-line treatment
- Electrical cardioversion for unstable patients or if pharmacological treatment fails
- In recurrent cases, temporary pacing to increase heart rate and shorten QT interval
Causes
- QT-prolonging medications (e.g., certain antiarrhythmics, antipsychotics, antibiotics)
- Electrolyte imbalances, especially hypokalemia and hypomagnesemia
- Bradycardia or long pauses in cardiac rhythm
- Structural heart disease, including ischemic heart disease and cardiomyopathies
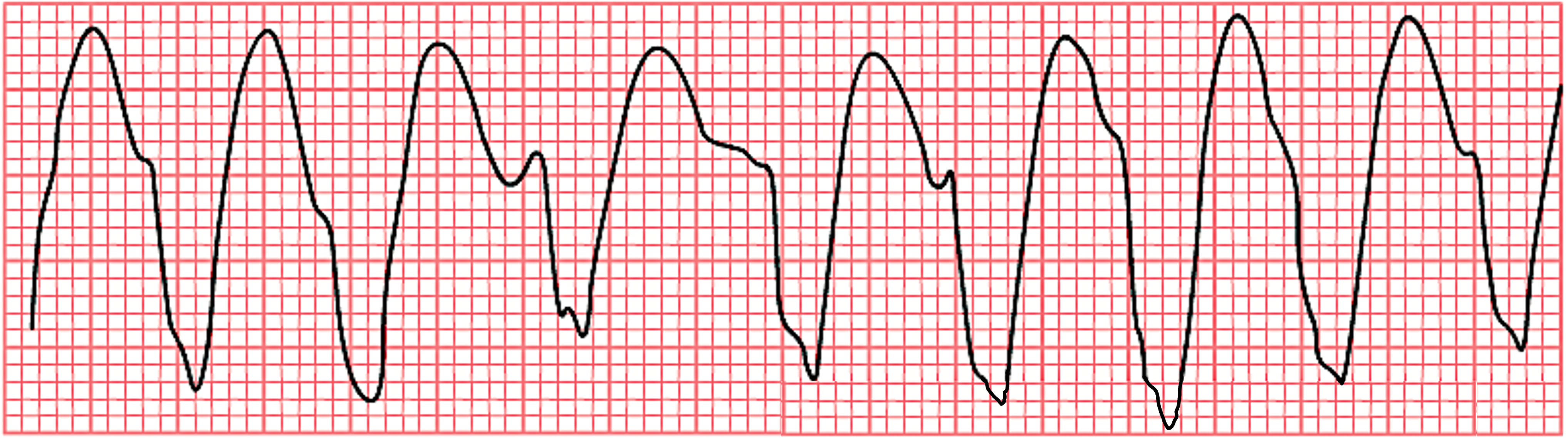
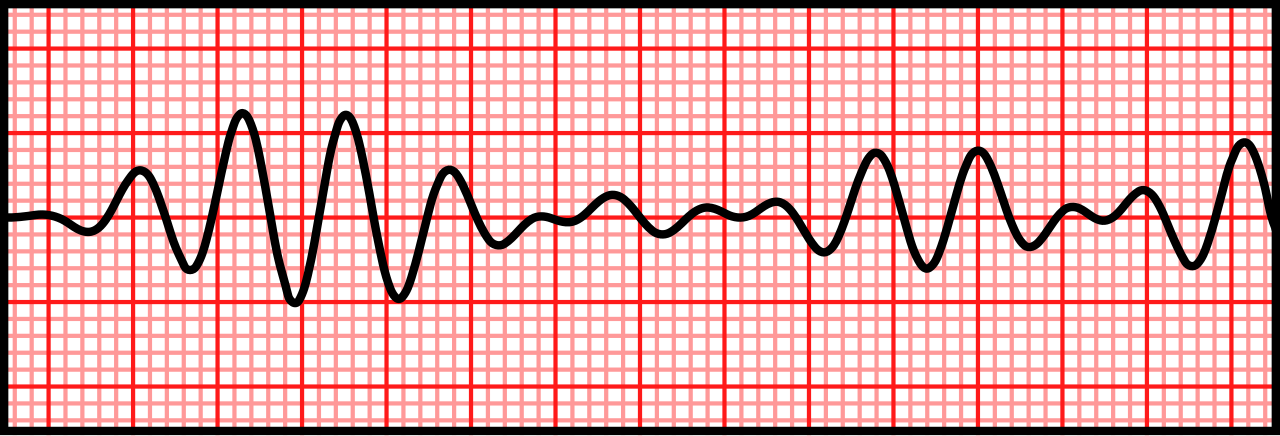
6. Ventricular Fibrillation
Characterized by rapid, chaotic electrical activity from multiple foci in the ventricles, ventricular fibrillation (V-fib) is a life-threatening cardiac arrhythmia and a type of cardiac arrest. It results in uncoordinated quivering of the ventricular myocardium instead of effective contractions that would squeeze the lower chambers of the heart for adequate ejection of blood, thus leading to a complete loss of cardiac output. Ventricular fibrillation is a medical emergency that requires immediate intervention to prevent mortality.
Characteristics of Ventricular Fibrillation
- Rhythm: Completely irregular, with no discernible pattern
- Rate: Impossible to determine. Chaotic electrical activity typically exceeds 300 bpm
- P wave: Not visible due to the chaotic ventricular activity
- PR interval: Not applicable due to absence of identifiable P waves and QRS complexes
- QRS complex: No identifiable QRS complexes
- Tolerance: Not tolerated; rapidly leads to loss of consciousness and cardiac arrest
Clinical Significance
- Represents a cardiac emergency requiring immediate defibrillation
- Without prompt treatment, leads to death within minutes
- Often the terminal rhythm in sudden cardiac death
Signs & Symptoms
- Sudden loss of consciousness
- Absences of pulse and breathing
- Unresponsiveness to stimuli
- Sudden collapse in witnessed cases
Treatment
- Immediate cardiopulmonary resuscitation (CPR) to maintain blood flow
- Early defibrillation, the definitive treatment for V-fib
- Advanced cardiac life support (ACLS) protocols, including epinephrine and antiarrhythmic drugs
- Post-resuscitation care, including addressing underling causes and considering implantable cardioverter defibrillator (ICD) placement
Causes
- Acute myocardial infarction
- Severe electrolyte imbalances, particularly hypokalemia or hyperkalemia
- Drug toxicity, including certain antiarrhythmic medications
- Cardiomyopathies and structural heart diseases
- Electrocution accidents
- Deterioration of other ventricular arrhythmias, including V-tach
7. Asystole
Often referred to as “flatline,” asystole is a state of no cardiac electrical activity, resulting in the absence of heart contractions. It represents the most severe form of cardiac arrest and is characterized by a flat line on the EKG. Asystole is a medical emergency requiring immediate intervention, as it is incompatible with life if prolonged. Importantly, asystole is not a “shockable” rhythm, and defibrillation is ineffective and potentially harmful in this condition. Defibrillation may only be considerable if asystole transitions into a shockable rhythm during CPR.
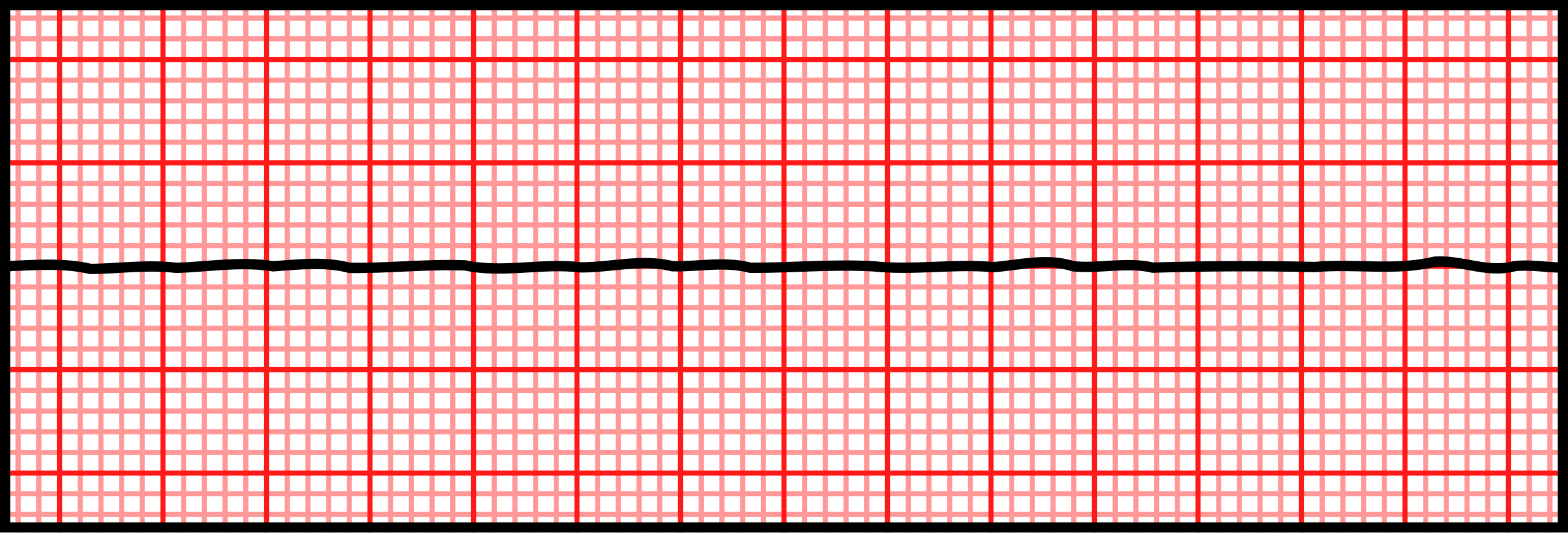
Clinical Significance
- Represents a dire medical emergency with extremely poor prognosis
- Often the terminal rhythm in prolonged cardiac arrest situations
- Requires immediate and aggressive resuscitation efforts, but not defibrillation
Signs & Symptoms
- Sudden loss of consciousness
- Absence of pulse and breathing
- Unresponsiveness to stimuli
- Pale or cyanotic skin color
Treatment
- Check status of patient and ensure all EKG leads are placed correctly with adequate skin contact
- Immediate high-quality CPR
- Administration of epinephrine as per ACLS protocols
- Identification and treatment of potentially reversible causes
- Consider transcutaneous pacing in specific situations
- Consider termination of efforts
- Defibrillation is ineffective
Causes
- Chest or direct heart trauma
- End-stage of other lethal arrhythmias (e.g., V-fib, pulseless electrical activity)
- Severe electrolyte imbalances, particularly hyperkalemia
- Massive myocardial infarction or severe heart failure
- Hypoxia, hypothermia, hypovolemia, or other severe systemic insults
- Drug overdose, particularly with cardiac medications
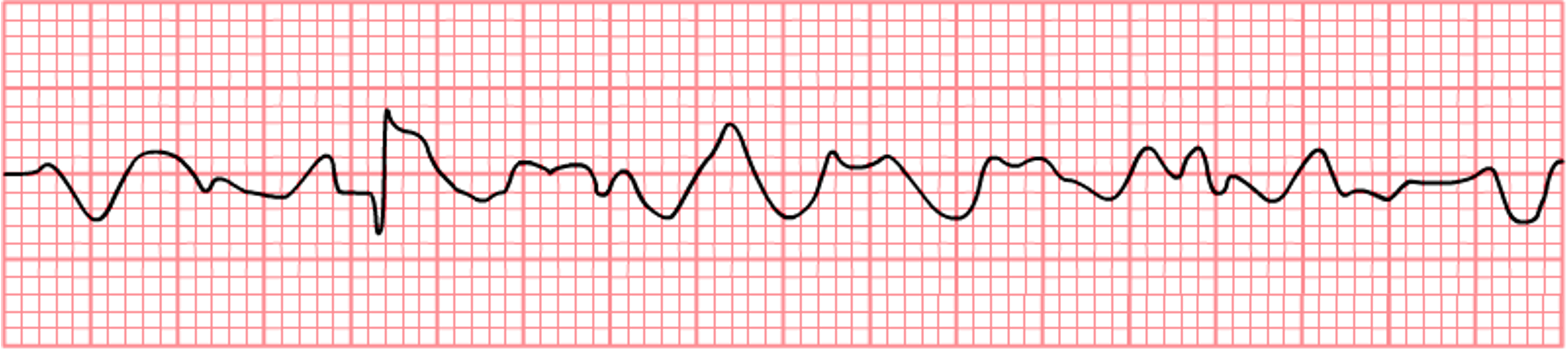
8. Pulseless Electrical Activity
Pulseless electrical activity (PEA) is a form of cardiac arrest characterized by organized electrical activity on the EKG without detectable mechanical cardiac output. In PEA, the heart’s electrical system continues to function, but the myocardium fails to contract effectively, resulting in the absence of a palpable pulse or measurable blood pressure. This condition represents a critical medical emergency requiring immediate intervention.
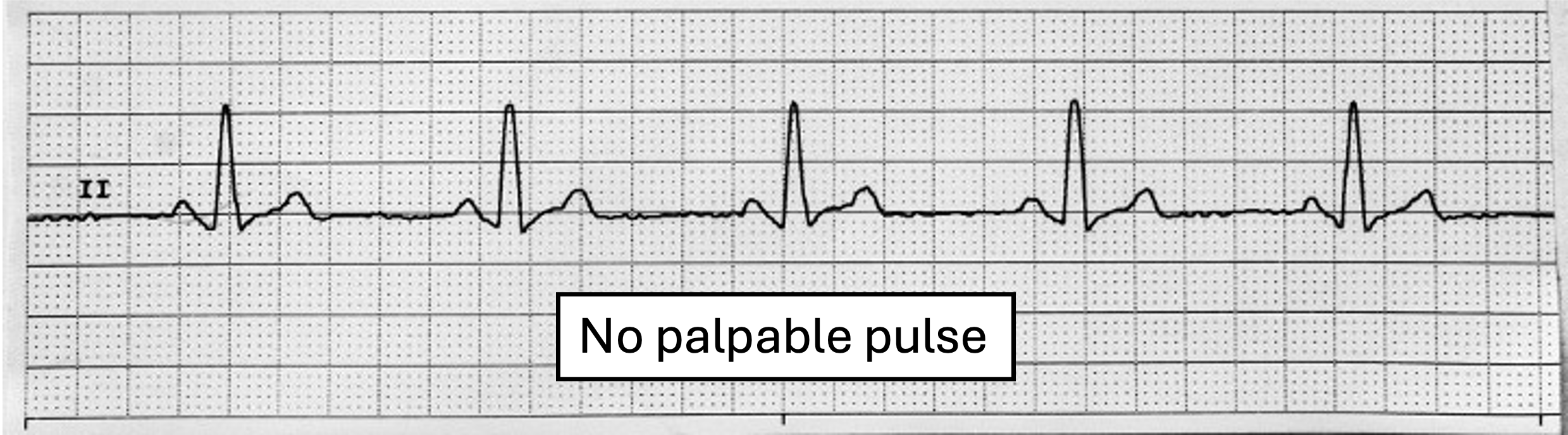
Characteristics of PEA
- Rhythm: Can be regular or irregular, depending on the underlying rhythm
- Rate: Variable, often between 30–100 bpm
- P wave: May be present, depending on the underlying rhythm
- PR interval: May be normal or prolonged if P waves are present
- QRS complex: Usually present and may appear normal or widened
- Tolerance: Not tolerated; results in immediate loss of consciousness and rapid EKG deterioration
Clinical Significance
- Indicates a severe, life-threatening condition with poor prognosis if not quickly reversed
- Requires immediate CPR and treatment of underlying causes
- Often a sign of significant systemic illness or severe cardiac compromise
Signs & Symptoms
- Sudden loss of unconsciousness
- Absence of palpable pulse despite visible EKG activity
- Cessation of breathing or gasping respiration
- Unresponsiveness to stimuli
Treatment
- Immediate high-quality CPR
- Rapid identification and treatment of reversible causes
- Administration of epinephrine as per ACLS protocols
- Consider other interventions based on suspected cause
Causes
- Hypovolemia, hypoxia, acidosis, hypokalemia, hyperkalemia, hypothermia
- Tension pneumothorax, cardiac tamponade, drug overdose, thrombosis (coronary or pulmonary)
- Massive myocardial infarction or end-stage heart failure
- Severe sepsis or other systemic illnesses causing shock
Image Attributions:
Fig. 7.1 – This work, “Ectopic focus (no title)“, is adapted from “Heart and electrical conduction system” by Jonas de Jong, used under CC BY-SA 3.0. “Ectopic focus (no title)” is licensed under CC BY-SA 4.0 by YitzhakNat
Fig. 7.2 – “Premature_Ventricular_Contraction” by Rocuronium Bromide. The image is dedicated to the public domain under CC0
Fig. 7.3 – This work is a derivate of “NSR with PVCs” by ECG Guru and is licensed under CC BY-NC-SA 4.0 / Brackets added above original
Fig. 7.4 – “NSR and Ectopic Beats (PVC and PAC)” by YitzhakNat is licensed under CC BY-SA 4.0
Fig. 7.5 – “Interpolated PVC’s” by Frank G. Yanowitz, M.D. in ECG Learning Center is licensed under CC BY-ND-NC 1.0
Fig. 7.6 – “Sinus with Unifocal PVCs” by Deanna Hoyord is licensed under CC BY 4.0
Fig. 7.7 – “Multifocal PVC” by Edward Burns and Robert Buttner is licensed under CC BY-NC-SA 4.0
Fig. 7.8 – “Premature Ventricular Complex PVC bigeminy” by Edward Burns and Robert Buttner is licensed under CC BY-NC-SA 4.0
Fig. 7.9 – This work is a derivate of “Electrocardiogram suggestive of PVCs originating from the RVOT” by Prousi, Davis, Feldman, and Siddique in ClinMed International Library and is licensed under CC BY 4.0 / Cropped from original, color shift, and added sharpness
Fig. 7.10 – This work is a derivate of “PVC pairs (couplets)” by Edward Burns and Robert Buttner and is licensed under CC BY-NC-SA 4.0 / cropped from original and sharpness added
Fig. 7.11 – “Non-sustained VT (NSVT)” by Edward Burns and Robert Buttner and is licensed under CC BY-NC-SA 4.0
Fig. 7.12 – This work is a derivate of “E000785 (CardioNetworks ECGpedia)” by CardioNetworks and is licensed under CC BY-SA 4.0 / Cropped from original
Fig. 7.13 – “St Elevation with R on T Phenomenon Converting to V-Tach” by Deanna Hoyord is licensed under CC BY 4.0
Fig. 7.14 – This work is a derivative of “Typical experimental ECG recordings showing the different arrhythmias taken into account by our model” by Casaleggio, Hines, and Migliore in PLOS One and is licensed under CC BY 4.0 / Created new titles and renamed “short VTs” from original to “Short runs of V-tach”
Fig. 7.15 – “Rhythm idioventricular” by ECGpedia is licensed CC BY-NC-SA 3.0 / Removed logo
Fig. 7.16 – “AIVR from the LV” by Jason E. Roediger is licensed under CC BY-SA 3.0 / Cropped from original
Fig. 7.17 – “Ventricular Tachycardia” by Rocuronium Bromide is dedicated to the public domain under CC0
Fig. 7.18 – “Test0001” by CardioNetworks is licensed under CC BY-SA 3.0 / Logo and title removed
Fig. 7.19 – “Torsades de Pointes (polymorphic VT)” by Rocuronium Bromide is dedicated to the public domain under CC0
Fig. 7.20 – “Torsades converted by AICD ECG strip Lead II” by Displaced is dedicated to the public domain under CC0 / Cropped from original and grayscaled
Fig. 7.21 – “Ventricular Fibrillation” by Rocuronium Bromide is dedicated to the public domain under CC0
Fig. 7.22 – “De-Rhythm ventricular fibrillation (CardioNetworks ECGpedia)” by CardioNetworks is licensed under CC BY-SA 3.0 / Removed logo and title
Fig. 7.23 – “Asystole” by Rocuronium Bromide is dedicated to the public domain under CC0
Fig. 7.24 – This work, “Pulseless electrical activity” is adapted from “Sinus Bradycardia” by Deanna Hoyord, used under CC BY 4.0. “Pulseless electrical activity” is licensed under CC BY-NC 4.0 by Dr. Joshua E. McGee
An abnormal pacemaker site that can interfere with the normal electrical impulses of the heart.