13 Pacemakers and Implantable Cardioverter Defibrillators
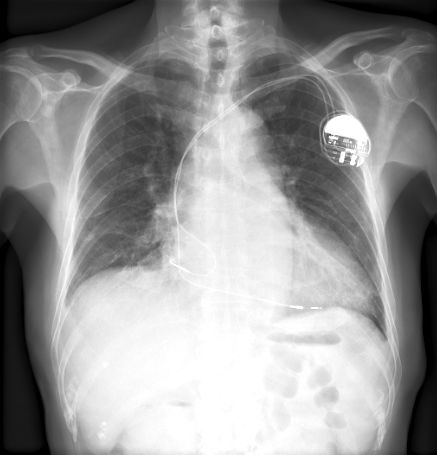
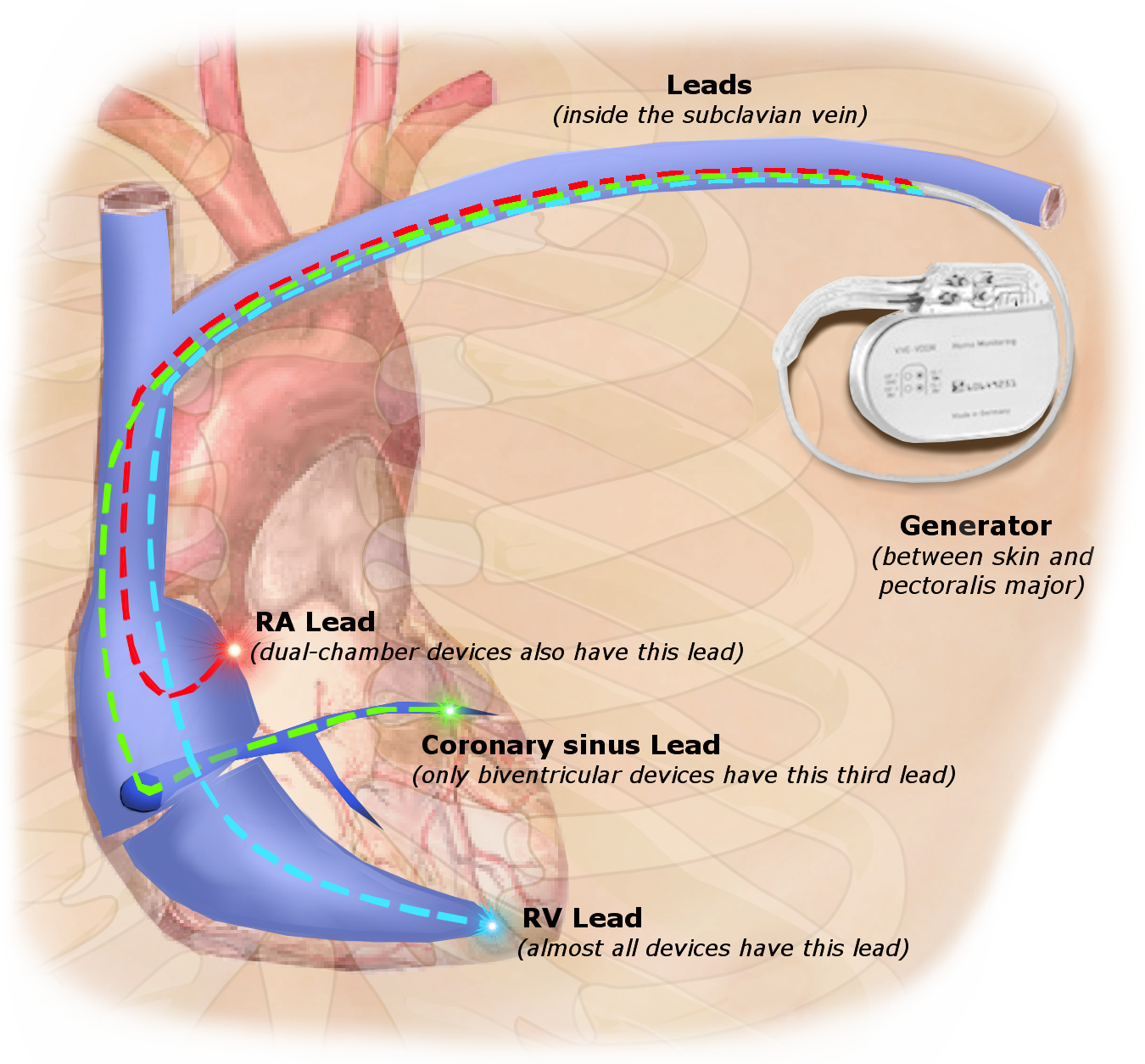
Pacemakers are electronic devices designed to regulate the heart’s rhythm by delivering electrical impulses to the myocardium. These devices are typically implanted in the chest and consist of a pulse generator and one or more leads with electrodes that connect to directly to a chamber of the heart. Pacemakers are used to ensure the heart beats at a normal rate and rhythm, especially in cases where the natural electrical conduction system is compromised, leading to slow or irregular rhythms.

Indications for Pacemaker Implantation
Pacemakers are implanted to manage various cardiac conditions that cause abnormal cardiac rhythms. Common indications include symptomatic bradycardia and certain heart blocks. Pacemakers are also used in some cases of heart failure and certain types of tachyarrhythmias to maintain a regular heart rhythm and improve cardiac function.
Types of Pacemakers
-
Permanent Pacemakers
- Implanted under the skin, usually near the collarbone, for long-term management of chronic arrhythmias
- Used to treat conditions like chronic AV block and sick sinus syndrome
-
Temporary Pacemakers
- Used for short-term pacing needs, often in hospital settings
- Indicated for acute conditions like post-surgical heart block or drug-induced bradycardia
Pacemaker Classification
-
Synchronous (Demand) Pacemakers
- Activate only when the heart’s natural rhythm falls below a preset rate
- Helps conserve battery life and maintain natural heart function when possible
-
Asynchronous (Fixed-Rate) Pacemakers
- Deliver impulses at a constant rate, regardless of the heart’s intrinsic activity
- Typically used in situations where the heart’s natural rhythm is unreliable or absent
Pacemaker Codes
-
AAI
- Atrial pacing, atrial sensing, inhibits artificial impulses if intrinsic atrial activity is detected
-
VVI
- Ventricular pacing, ventricular sensing, inhibits artificial impulses if intrinsic ventricular activity is detected
-
DVI
- Dual-chamber pacing, ventricular sensing, inhibits artificial impulses if intrinsic ventricular activity is detected
-
VDD
- Ventricular pacing, dual-chamber sensing, allows for atrioventricular synchrony without directly pacing the atrium
-
DDD
- Dual-chamber pacing and sensing, can both inhibit and trigger pacing based on intrinsic atrial and ventricular activity
-
DDDR
- Dual-chamber pacing and sensing, also includes rate modulation to adjust pacing rate based on physical activity
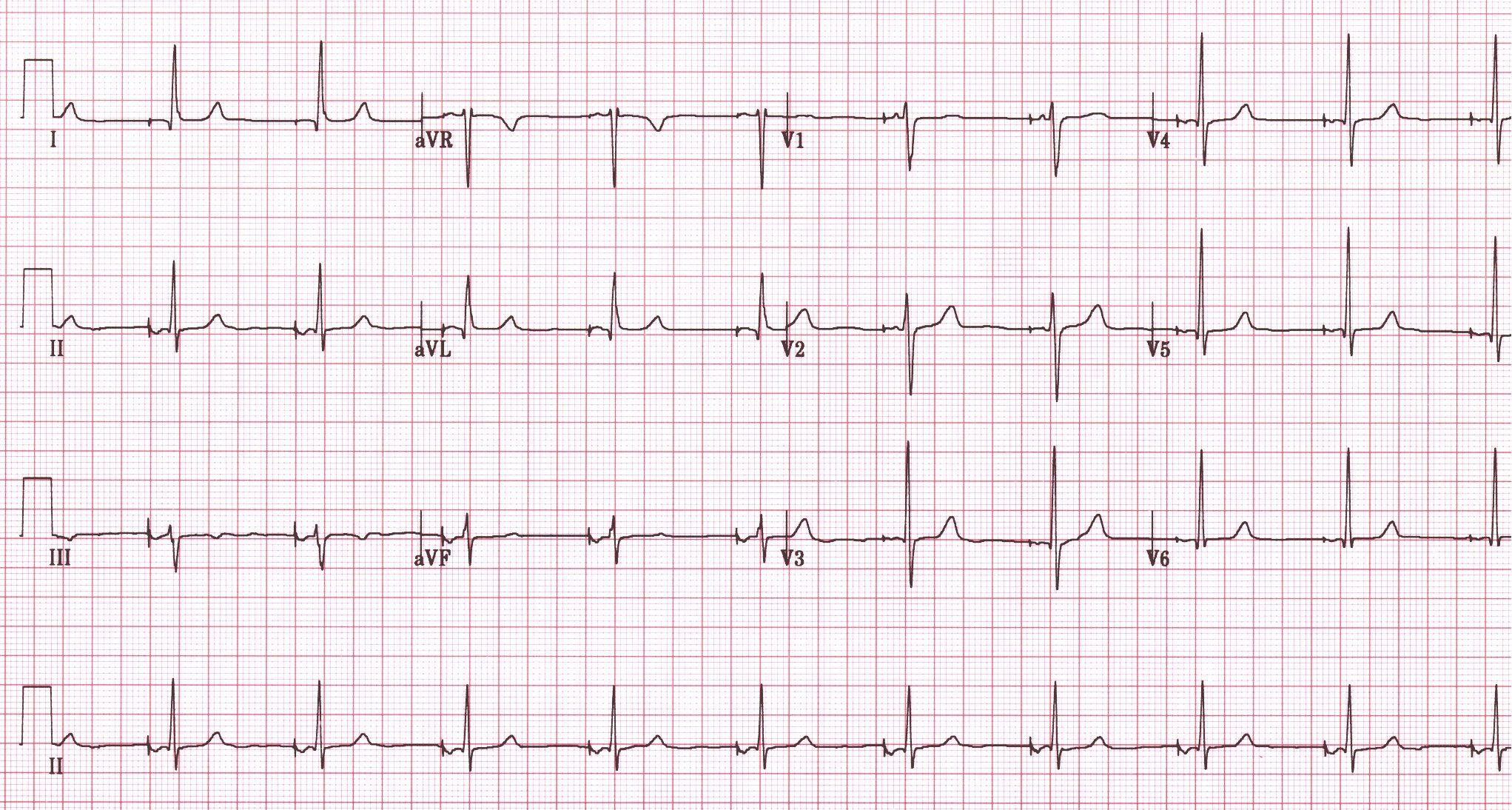
EKG Changes with Pacemakers
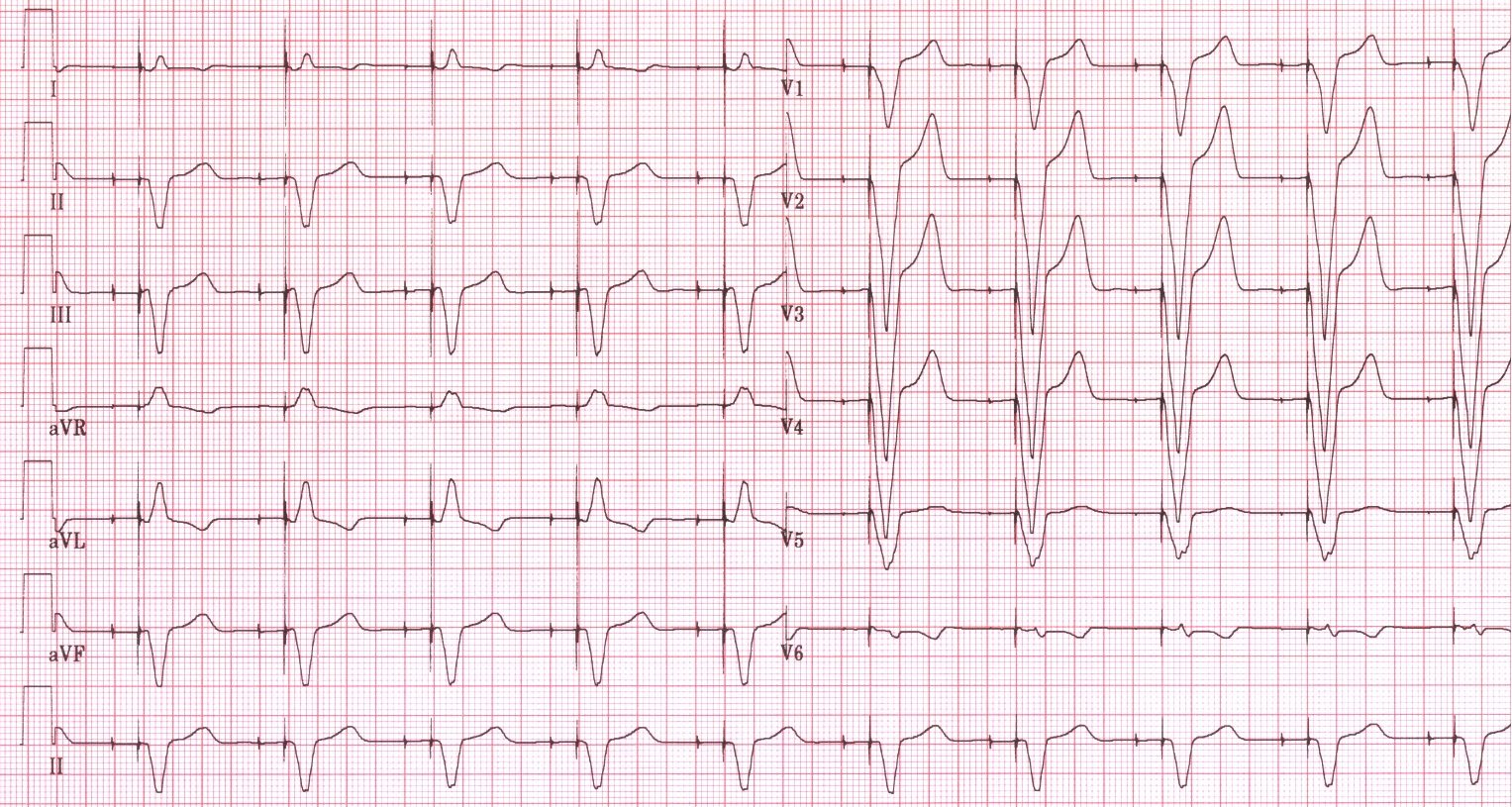
On the EKG, pacemaker activity is characterized by distinct vertical spikes, known as pacemaker spikes or pacing spikes, which precede the paced chamber’s depolarization. In ventricular pacing, a pacemaker spike is followed by a wide QRS complex, indicating artificial ventricular depolarization. Atrial pacing shows a spike before the P wave. Dual-chamber pacemakers, which involves leads placed in the right atrium and right ventricle, produce spikes before both the P wave and QRS complex. These changes help identify the type of pacemaker and its functioning.
-
Pacemaker Spikes
- Vertical spikes on the EKG represent the electrical activity of the artificial pacemaker
-
Atrial Pacing
- A pacemaker spike precedes the P wave
- P wave morphology depends on lead placement, as it could appear biphasic, inverted, or have low amplitude, but may appear normal if the pacing lead is positioned appropriately
-
Ventricular Pacing
- A pacemaker spike precedes the QRS complex
- Wide QRS complexes
- Right ventricular pacing typically results in a QRS morphology similar to a LBBB
- Left ventricular pacing can resemble QRS morphology found in RBBB
- QRS complexes should be discordant with the following ST segments and T waves
-
Dual-Chamber Pacing
- Artificial pacing of both the atrium and ventricle results in pacemaker spikes before the P wave and the QRS complex
Problems with Pacemakers
-
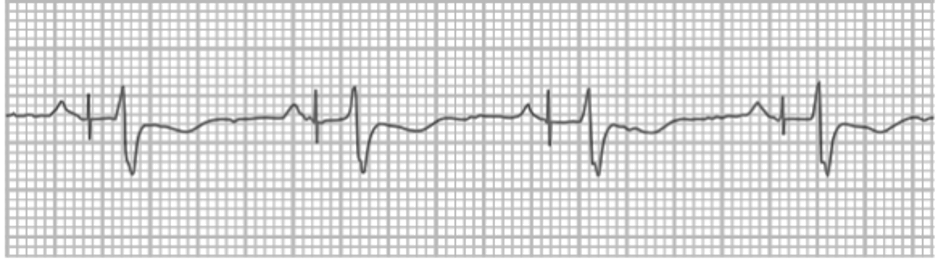
Failure to Capture
- Occurs when the electrical impulse of the pacemaker fails to depolarize the myocardium
- May be due to lead displacement, battery depletion, or increased pacing threshold
-
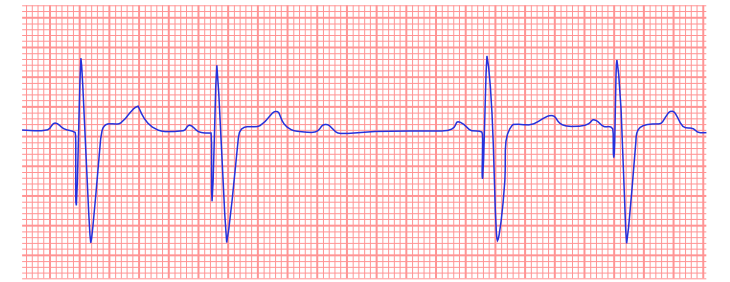
Sensing Malfunction
- The pacemaker fails to detect intrinsic cardiac activity, leading to inappropriate pacing
- Can be caused by lead issues, interference, or incorrect sensitivity settings
Implantable Cardioverter Defibrillators
A pacemaker and an implantable cardioverter defibrillator (ICD) are both devices used to manage arrhythmias, but they serve different purposes. While both are implanted under the skin to regulate cardiac rhythms, a pacemaker primarily delivers low-energy electrical impulses to maintain a steady rate, addressing issues like bradycardia or irregular rates. In contrast, an ICD monitors the heart for dangerously fast rhythms and can deliver both low-level pacing and high-energy shocks to restore normal rhythm during life-threatening arrhythmias, such as ventricular fibrillation. An ICD is recommended for patients who have experienced cardiac arrest or are at high risk of sudden cardiac death due to cardiac issues. It is important to know that patients with ICDs need to be careful around devices with strong magnets and should consult their doctor about safe exercise and lifestyle choices.
Image Attributions:
Fig. 13.1 – “St Jude Medical pacemaker in hand” by Steven Fruitsmaak is licensed under CC BY 3.0
Fig. 13.2 – “Chest xray pacemaker” by Jonas de Jong is licensed under CC BY-NC-SA 4.0
Fig. 13.3 – “PPM” by Nicholas Patchett is licensed under CC BY-SA 4.0
Fig. 13.4 – “DVA0838” by W.G. de Voogt, used under CC BY-NC-SA 3.0 / Cropped from original
Fig. 13.5 – “DVA0856” by W. G. de Voogt, used under CC BY-NC-SA 3.0 / Cropped from original
Fig. 13.6 – “Atrial malsensing” by Jonas de Jong, used under CC BY-NC-SA 4.0 / Cropped from original and grayscaled
Fig. 13.7 – “Ventricular oversensing” by Jonas de Jong, used under CC BY-NC-SA 4.0