12 Bundle Branch Blocks and Hemiblocks
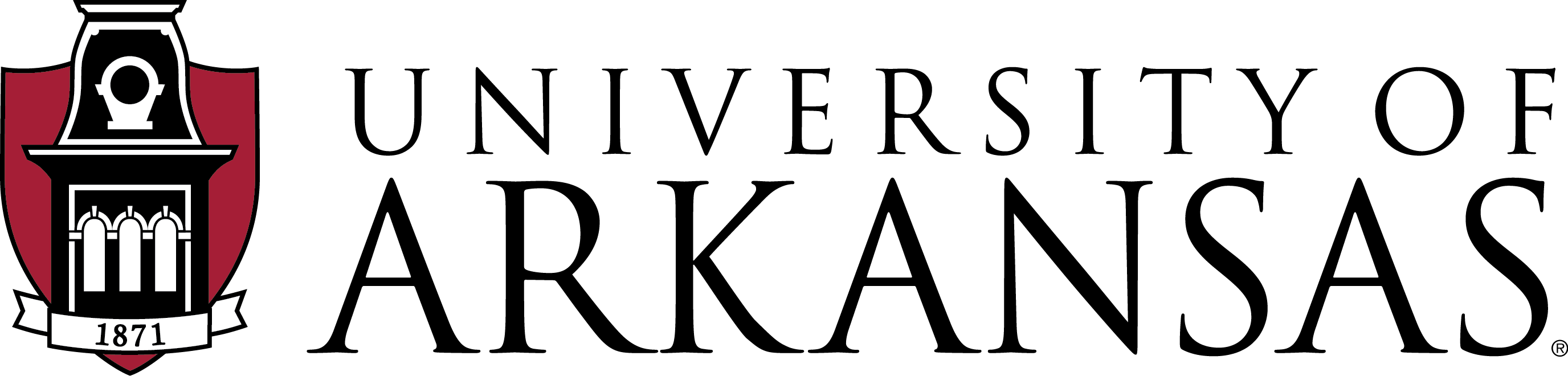
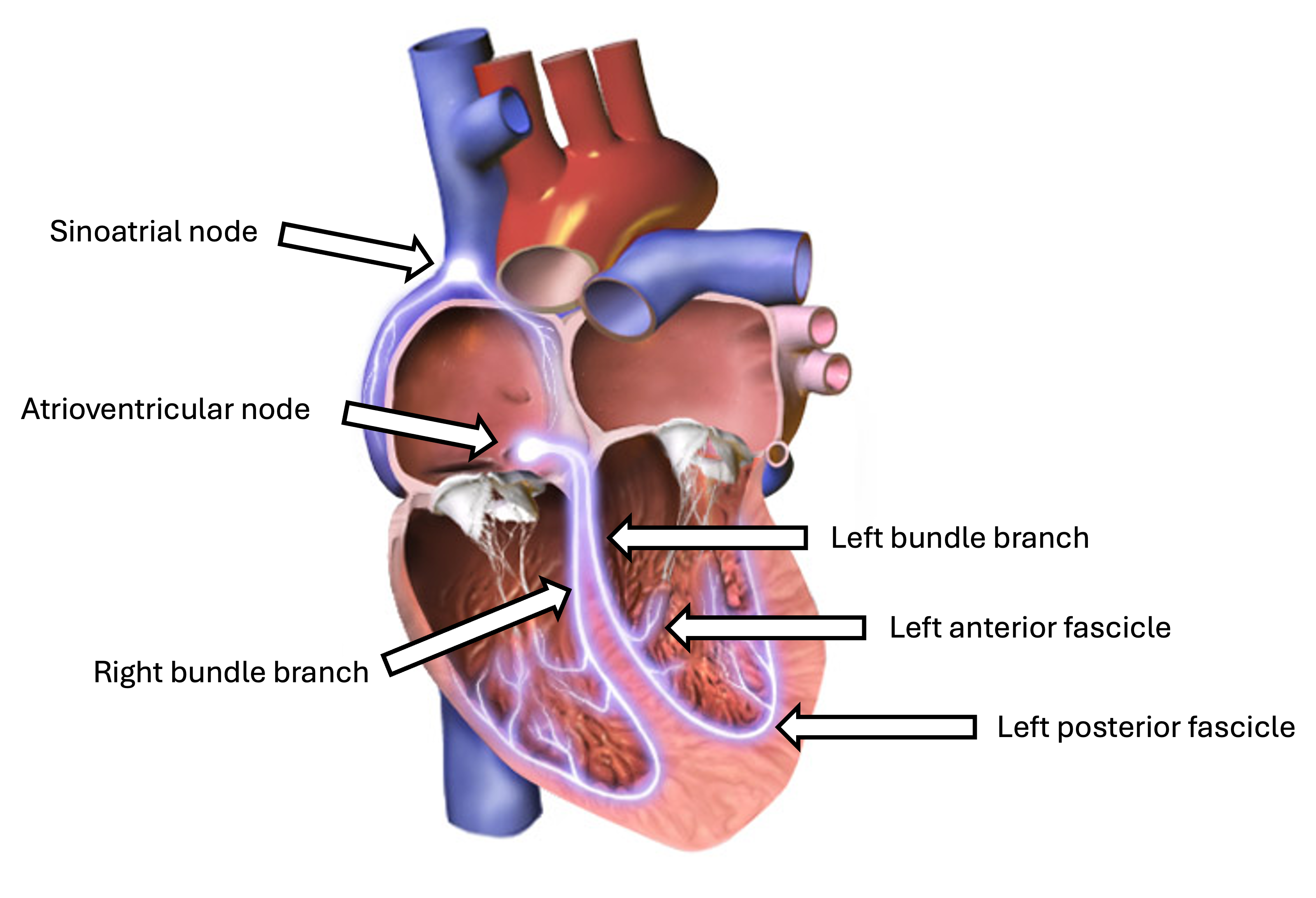
Bundle branch blocks and hemiblocks are conduction abnormalities that affect the heart’s electrical system, specifically the bundle of His and its branches. These conditions can alter the normal sequence of ventricular depolarization, leading to characteristic changes on the EKG. These are diagnosed by observing the width and configuration of the QRS. Understanding these patterns is crucial for accurate EKG interpretation and patient management.
1. Left Bundle Branch Block
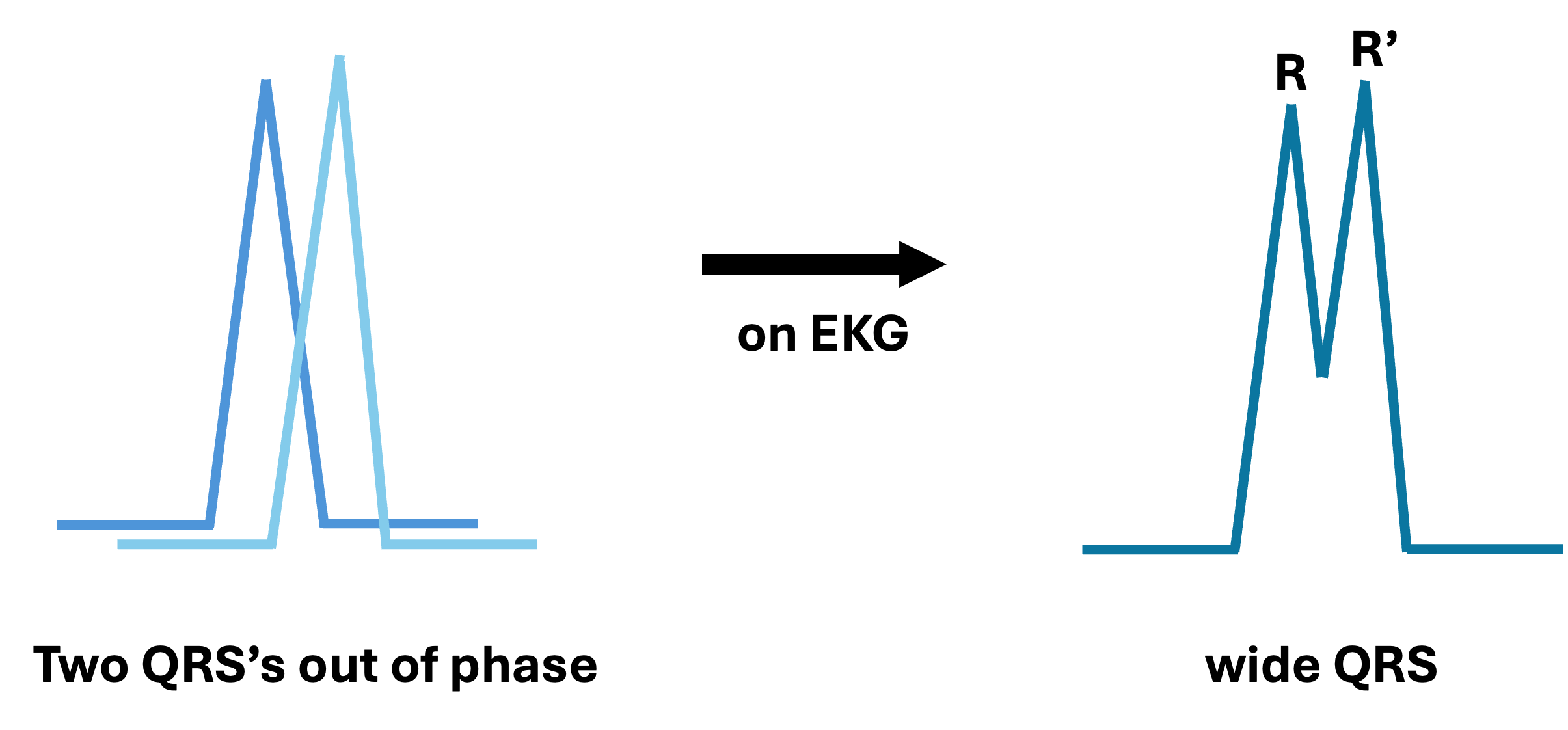
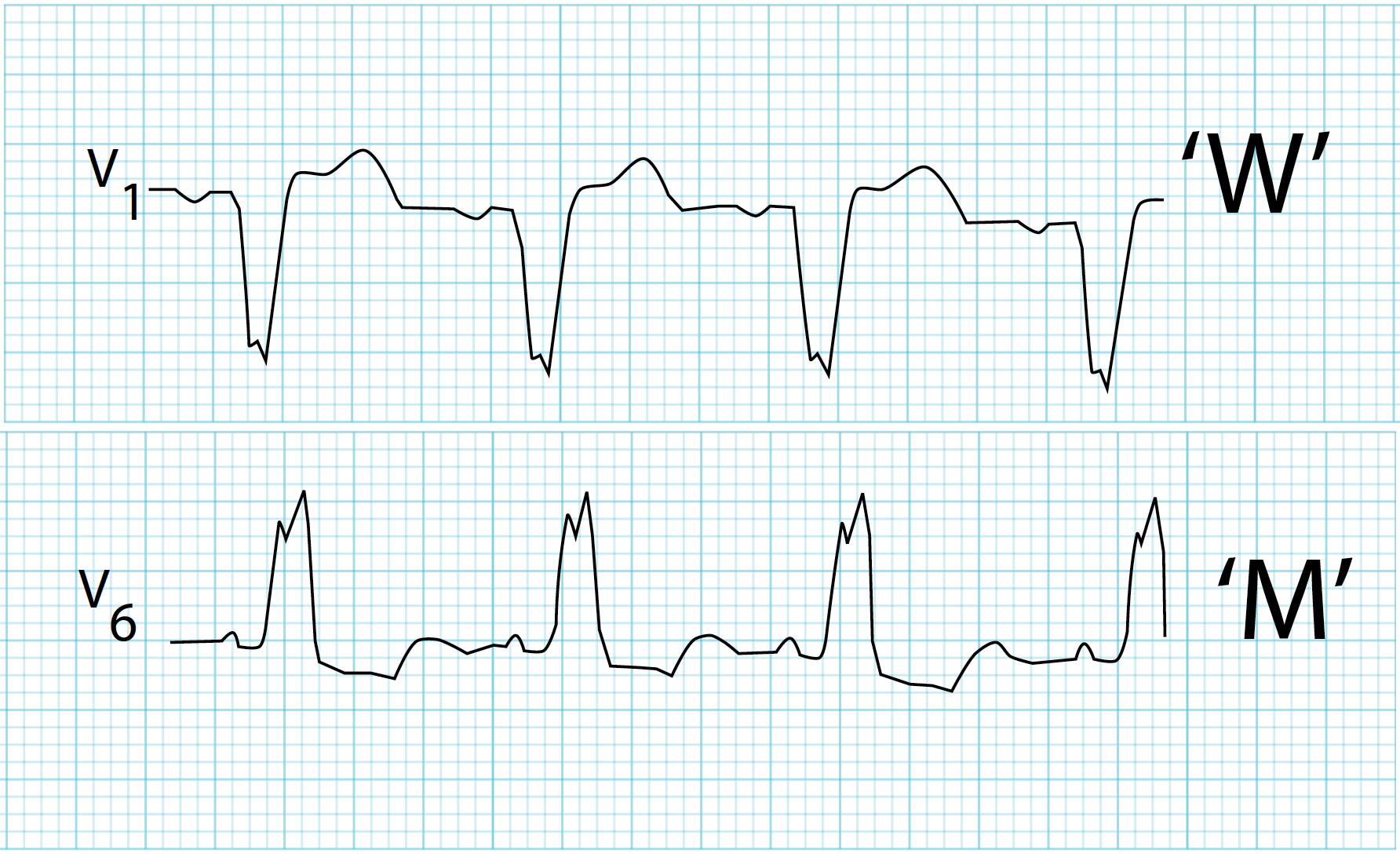
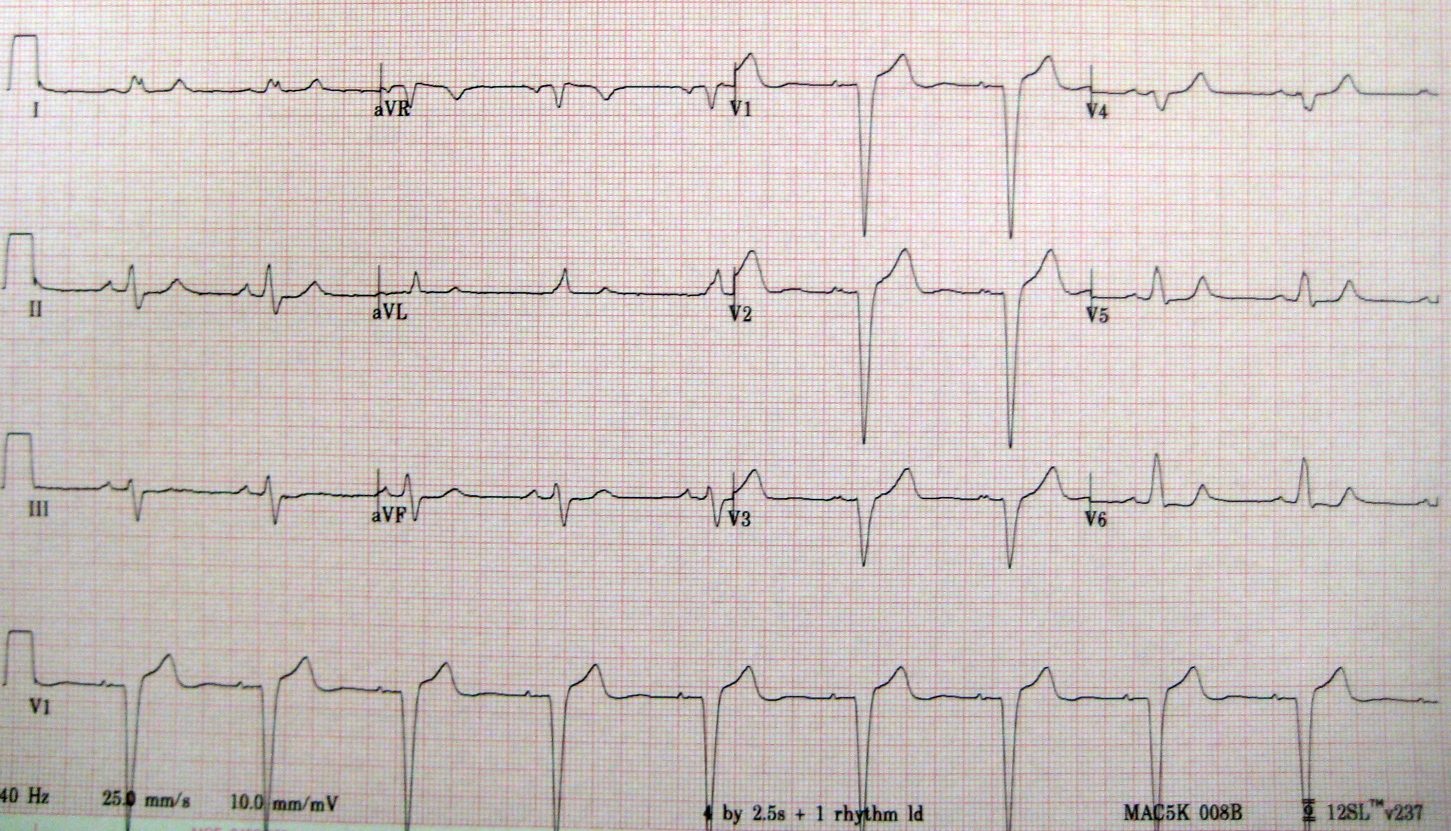
A left bundle branch block (LBBB) occurs when conduction through the left bundle branch is impaired or blocked. This results in an altered sequence of ventricular depolarization, with the right ventricle activating before the left ventricle, characterized by tall, wide R waves in the lateral leads (I, aVL, V5, V6) and deep S waves in the right precordial leads (V1 – V3). The delay between the right and left ventricles creates distinctive “M-shaped” R waves in the lateral leads, a hallmark of LBBB. Because the delay makes impulses travel first through the right bundle branch to the right ventricle and then to the left ventricle through the septum, this reverses the normal septal activation direction and, thus, removes the lateral Q waves.
Criteria for LBBB interpretation:
- QRS complex
- Duration ≥0.12 secs
- Wide and often notched or slurred appearance
- Dominant S wave in V1 and V2
- R waves in lateral leads
- Broad, monophasic R waves in leads I, aVL, V5, V6
- Often notched or “M-shaped” appearance
- R wave peak time >0.06 secs in leads V5 and V6
- Q waves
- Absent in lateral leads
- Axis deviation
- Left axis deviation is often present in LBBB, but is not a diagnostic criterion
Distinguishing ST elevation from MI and LBBB
- Discordant ST elevation
- ST elevation can occur in LBBB, but is usually discordant, meaning the ST segment deflection is in the opposite direction of the QRS complex.
- For example, if the QRS complex is predominantly negative, the ST segment may show elevation in LBBB. Whereas, ST elevation in a STEMI is usually concordant with the QRS complex.
- ST elevation can occur in LBBB, but is usually discordant, meaning the ST segment deflection is in the opposite direction of the QRS complex.
- Proportionate elevation
- The degree of ST elevation in LBBB is typically <25% of the depth of the preceding S wave, which can help distinguish it from true myocardial infarction.
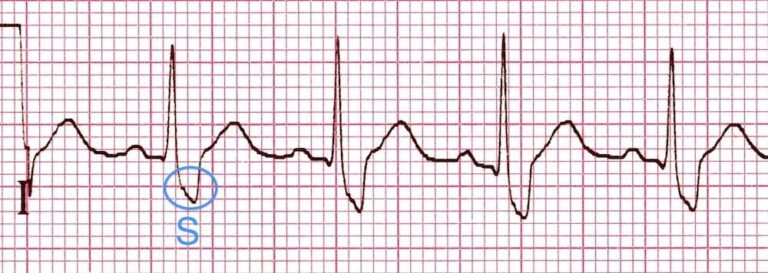
- Smith-Modified Sgarbossa Criteria
- If any one of the following Smith-Modified Sgarbossa Criteria[1] is met, it indicates a high likelihood of STEMI rather than changes solely due to LBBB:
- Concordant ST elevation
- One or more leads with a positive QRS complex that has concordant ST elevation of ≥1 mm
- Concordant ST depression
- One or more leads from V1 – V3 that has ≥1 mm of concordant ST depression
- Excessively discordant ST elevation
- One or more leads with ≥1 mm ST elevation and proportionally excessive discordant ST elevation, as defined by ST segment elevation ≥25% of the depth of the preceding S wave
- Concordant ST elevation
- If any one of the following Smith-Modified Sgarbossa Criteria[1] is met, it indicates a high likelihood of STEMI rather than changes solely due to LBBB:
Clinical Significance
- May indicate underlying heart disease (e.g., coronary artery disease, cardiomyopathy)
- Can mask signs of acute MI on EKG
- Associated with increased risk of heart failure and mortality
Signs & Symptoms
- Often asymptomatic
- May experience reduced exercise tolerance or dyspnea on exertion
- Symptoms related to underlying cardiac condition, if present
Treatment
- No specific treatment for LBBB itself
- Management focuses on treating the underlying condition with regular follow-up and monitoring for potential complications
- In some cases, cardiac resynchronization therapy may be considered
Causes
- Anterior MI
- Coronary artery disease
- Hypertension
- Cardiomyopathy
- Degenerative conduction system disease
- Valvular heart disease
- Hyperkalemia and digoxin toxicity
2. Right Bundle Branch Block
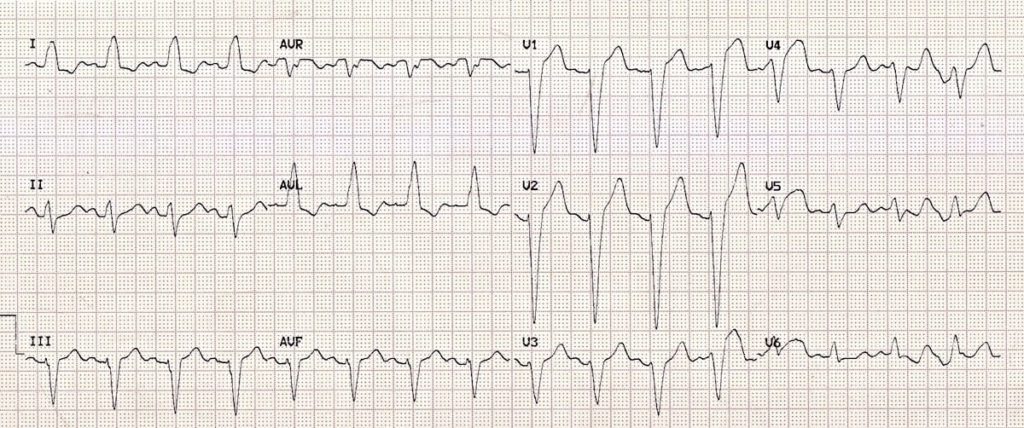
A right bundle branch block (RBBB) occurs when conduction through the right bundle branch is impaired or blocked, leading to delayed activation of the right ventricle.

Criteria for RBBB interpretation:
- QRS complex
- Duration ≥0.12 secs
- Broad morphology and often notched or slurred appearance
- A rule of thumb to differentiate between LBBB and RBBB is if there is a positive QRS deflection in lead V1, it is a RBBB, if negative, it is a LBBB.
- R waves in leads V1 and V2
- RSR’ pattern (“rabbit ears”) or “M-shaped” R waves in leads V1 and V2
- Tall, prominent R waves in leads V1 and V2
- S waves in lateral leads
- Wide, slurred S waves in leads I, aVL, V5, and V6
- Discordant ST segment changes
- ST depression or elevation in opposite direction of the preceding QRS complex
- ST depression often seen in leads V1, V2, and V3
- T wave
- Inverted T waves can be found in leads V1, V2, and V3
- Typically discordant, in the opposite direction of the QRS deflection
- Additional potential EKG changes
- Presence of a terminal R wave (or R’) in lead aVR
- Prolonged R wave peak time in right precordial leads


Clinical Significance
- May indicate underlying heart disease such as ischemic heart disease, pulmonary embolism, or congenital heart defects
- Can be associated with increased risk of arrhythmias and adverse cardiovascular events
Signs & Symptoms
- Often many patients with RBBB are asymptomatic
- If present, symptoms are usually related to the underlying cardiac or pulmonary condition
Treatment
- No specific treatment for RBBB itself
- Management focuses on treating the underlying condition with regular follow-up and monitoring for potential complications
- In some cases, cardiac resynchronization therapy may be considered
Causes
- Right ventricular hypertrophy
- Coronary artery disease
- Pulmonary conditions, such as pulmonary embolism or COPD
- Congenital heart defects
- Degenerative conduction system disease
3. Left Anterior Hemiblock
Hemiblocks, also known as fascicular blocks, are conduction disturbances affecting the left anterior or posterior fascicles of the left bundle branch. They can occur in isolation or in combination with other conduction abnormalities, including RBBB. Left anterior hemiblocks occur when the anterior fascicle of the left bundle branch is unable to conduct electrical impulses. This results in characteristic changes on the EKG:
Criteria for Left Anterior Hemiblock Interpretation:
- Left axis deviation
- Mean electrical axis is shifted to the left, typically between –45º and –90º
- Usually present, but can be less pronounced (between –30º and –45º), leading a probable diagnosis
- QRS complex
- Usually normal or slightly prolonged, but less than 0.12 secs
- R waves in lateral leads
- Presence of qR pattern in leads I and aVL, characterized by small Q waves followed by tall R waves
- Prolonged R wave peak time in lead aVL (>0.04 secs), indicating delayed conduction
- S waves in inferior leads
- Presence of rS complexes in leads II, III, and aVF, with small R waves and deep S waves
- Exclusion of other causes of left axis deviation
- It is important to rule out left ventricular hypertrophy and other potential causes of left axis deviation through clinical evaluation and additional imaging if necessary
- e.g., LBBB, inferior MI, Wolff-Parkinson-White syndrome
- It is important to rule out left ventricular hypertrophy and other potential causes of left axis deviation through clinical evaluation and additional imaging if necessary
Clinical Significance
- Often considered a benign finding but can indicate underlying heart disease such as MI, coronary artery disease, or cardiomyopathy
- May be associated with elevated risk of atrial fibrillation, heart failure, and mortality, especially in older patients
Signs & Symptoms
- Typically asymptomatic and is often discovered incidentally during routine EKGs
- Symptoms, if present, are usually related to the underlying cardiac condition rather than the block itself
Treatment
- No specific treatment is required for a left anterior hemiblock itself
- Management focuses on addressing any underlying cardiac conditions
Causes
- Can occur in healthy individuals
- More commonly associated with conditions like MI, coronary artery disease, left ventricular hypertrophy, and cardiomyopathy
4. Left Posterior Hemiblock
A rare conduction abnormality, also known as a left posterior fascicular block, that affects the posterior fascicle of the left bundle branch. Specific changes on the EKG are described below:
Criteria for Left Posterior Hemiblock Interpretation:
- Right axis deviation
- Mean electrical axis shifts to the right, typically between +90º and +180º
- Key diagnostic feature that occurs due to the posterior fascicle’s block causing the impulse to travel through the anterior fascicle, resulting in altered depolarization pattern
- QRS complex
- Usually normal or slightly prolonged, but less than 0.12 secs
- Presence of rS complexes in leads I and aVL
- Presence of qR complexes in leads II, III, and aVF
- Prolonged R wave peak time
- Increased R wave peak time in lead aVF, typically greater than 0.04 secs
- Exclusion of other causes of right axis deviation
- It is important to rule out right ventricular hypertrophy and other potential causes of right axis deviation through clinical evaluation and additional imaging if necessary
- e.g., lateral MI, COPD, hyperkalemia, Wolff-Parkinson-White syndrome, pulmonary embolus
- It is important to rule out right ventricular hypertrophy and other potential causes of right axis deviation through clinical evaluation and additional imaging if necessary
Clinical Significance
- Left posterior hemiblock is rare and often indicates significant myocardial damage
- Can occur with other blocks, increasing the risk of third degree heart block
Signs & Symptoms
- Often found incidentally, with symptoms usually related to underlying conditions
Treatment
- Focus is on managing underlying cardiac conditions
- Regular follow-up is important, especially with other conduction issues
Causes
- Often linked to coronary artery disease or MI
- Conditions like cardiomyopathy can lead to left posterior hemiblock
5. Bifascicular Block
A bifascicular block involves a conduction delay in two of the heart’s three fascicles. Specifically, it combines a RBBB with either a left anterior hemiblock or left posterior hemiblock. This condition can affect the cardiac electrical signaling, potentially leading to arrhythmias or a slower heart rate. It is often associated with structural heart disease and raises the risk of progressing to a third-degree heart block if further conduction damage occurs.
Criteria for Bifascicular Block:
- Meets criteria for RBBB
- Additionally meets criteria for either left anterior hemiblock or left posterior hemiblock
6. Trifascicular Block
A trifascicular block describes a bifascicular block combined with a first-degree AV block. Although “trifascicular block” suggests involvement of all three pathways, it does not mean complete blockage, which would result in a third-degree heart block. Instead, it indicates delays in the right bundle branch, one of the left fascicles, and the AV node. This condition signals significant conduction system disease and may necessitate interventions like pacemaker implantation, especially if symptoms are present or there is a risk of progression to complete heart block.
Criteria for Trifascicular Block:
- Meets criteria for first-degree AV block
- Meets criteria for RBBB
- Additionally meets criteria for either left anterior hemiblock or left posterior hemiblock
Remember that these conduction abnormalities can have significant clinical implications and may be associated with underlying heart disease. Always interpret EKG findings in the context of the patient’s clinical presentation and history.
Image Attributions:
Fig. 12.1 – “Heart Bundle Branches” by Bruce Blaus, is licensed under CC BY-SA 4.0 / Added labels
Fig. 12.2 – “QRS complex characteristics of left bundle branch block in leads V1 and V6” by Joshua E. McGee, is licensed under CC BY-NC 4.0
Fig. 12.3 – This work, “LBBB lateral lead QRS morphology”, is adapted from “LBBB QRS morphology notched R wave,” “LBBB QRS morphology M shaped,” “LBBB QRS morphology RS complex,” and “LBBB QRS morphology monophasic R wave” by Robert Buttner and Ed Burns, used under CC BY-NC-SA 4.0. “LBBB lateral lead QRS morphology” is licensed under CC BY-NC 4.0 by Joshua E. McGee
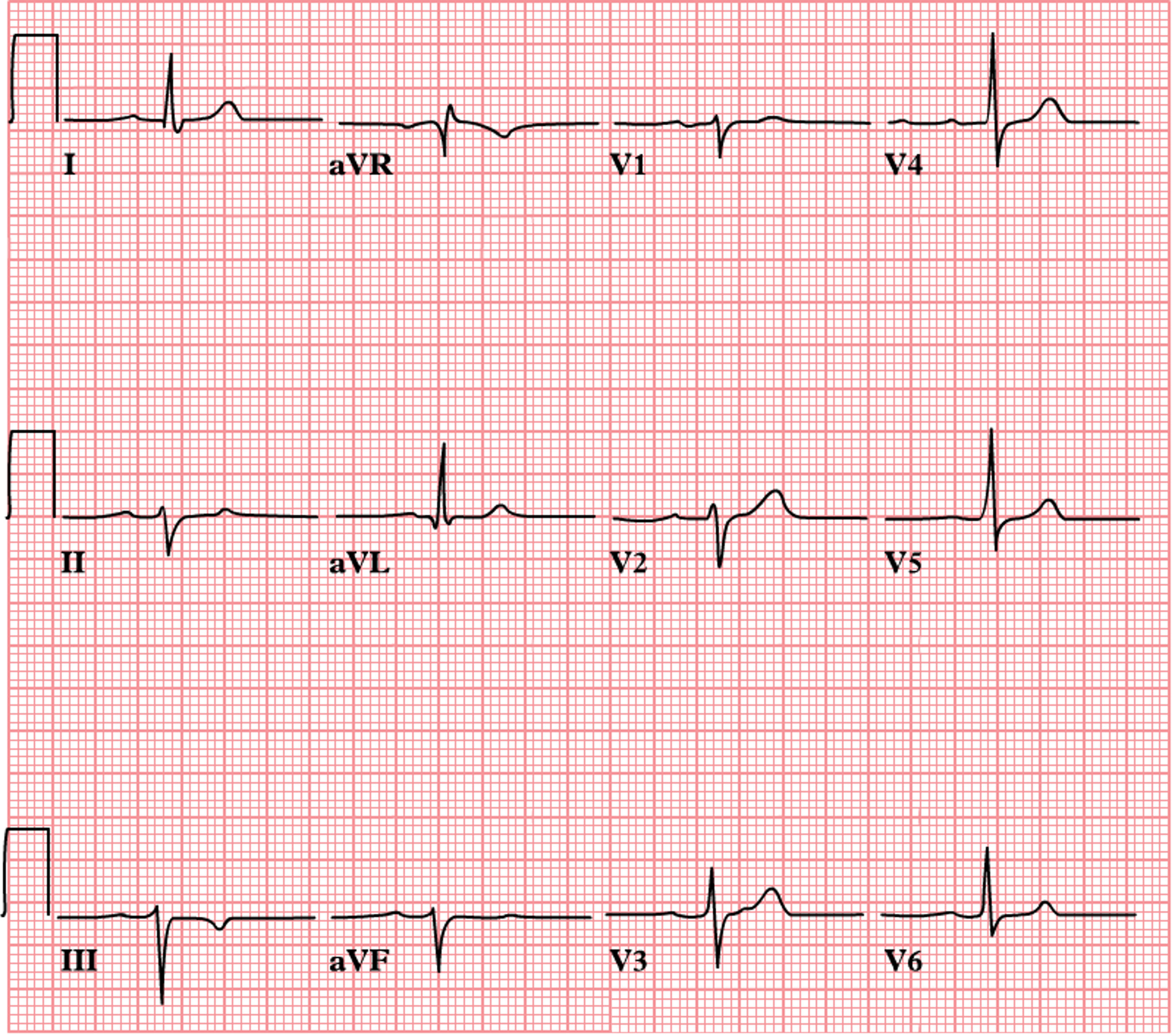
Fig. 12.4 – “Left Bundle Branch Block LBBB ECG Strip LITFL” by Robert Buttner and Ed Burns is licensed under CC BY-NC-SA 4.0
Fig. 12.5 – “LBBB2009” by James Heilman, is licensed under CC BY-SA 3.0 / Cropped from original
Fig. 12.6 – “ECG Left Bundle Branch Block LBBB” by Robert Buttner and Ed Burns, is licensed under CC BY-NC-SA 4.0
Fig. 12.7 – This work, “Right bundle branch block (RBBB) of the human heart,” is adapted from “Heart and electrical conduction system” by Jonas de Jong, used under CC BY-SA 3.0. “Right bundle branch block (RBBB) of the human heart” is licensed under CC BY-SA 4.0 by YitzhakNat
Fig. 12.8 – “ECG-Right-Bundle-Branch-Block-RBBB-V1-RSR-Complex” by Ed Burns and Robert Buttner, is licensed under CC BY-NC-SA 4.0
Fig. 12.9 – “ECG-Right-Bundle-Branch-Block-RBBB-Lead-I-wide-S-768×273” by Ed Burns and Robert Buttner, is licensed under CC BY-NC-SA 4.0
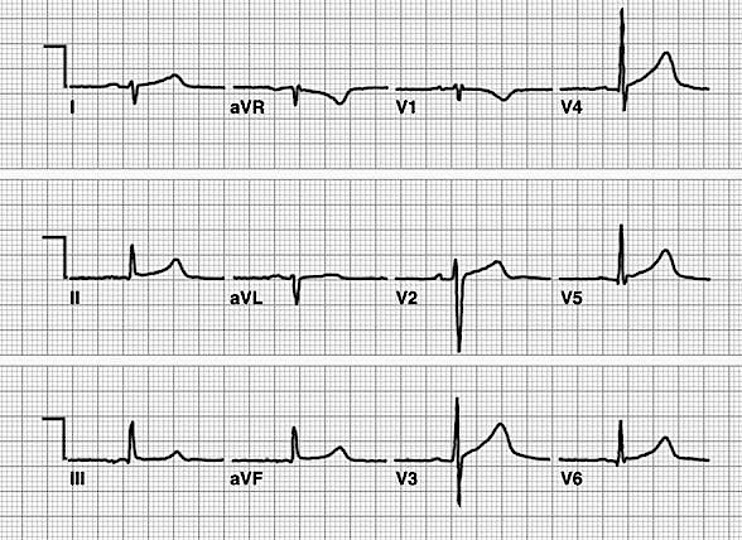
Fig. 12.10 – “Right Bundle Branch Block RBBB ECG Strip LITFL” by Ed Burns and Robert Buttner is licensed under CC BY-NC-SA 4.0
Fig. 12.11 – “LAHB” by Jonas de Jong, is licensed under CC BY-NC-SA 4.0 / Removed logo
Fig. 12.12 – “Left-Posterior-Fascicular-Block-LPFB-3” by John Larkin and Robert Buttner is licensed under CC BY-NC-SA 4.0 / Increased image sharpness
- Diagnosis of ST-elevation myocardial infarction in the presence of left bundle branch block with the ST-elevation to S-wave ratio in a modified Sgarbossa rule. Smith SW, Dodd KW, Henry TD, Dvorak DM, and Pearce LA. Annals of Emergency Medicine. ↵