8 Atrioventricular Blocks
The heart’s electrical system is an intricate network that ensures coordinated contraction of the atria and ventricles. At the core of this vital system is the atrioventricular (AV) node, a crucial gateway for electrical impulses traveling from the atria to the ventricles. Disruptions in this conduction pathway can lead to a group of conditions called AV blocks. These conduction issues can manifest in different degrees, ranging from slight delays to complete interruption of electrical signals between the upper and lower chambers of the heart. The severity of AV blocks can vary widely, from asymptomatic presentations to potentially life-threatening conditions, depending on the degree of block and the patient’s underlying cardiac function. AV blocks are classified into three main types: first-degree, second-degree (with two subtypes), and third-degree, each showing specific patterns on the EKG.
1. First-Degree Block
The mildest form of AV conduction disturbance is known as first-degree AV block. This condition is characterized by a delay in the transmission of electrical impulses from the atria to the ventricles, resulting in a prolonged PR interval on the EKG. Despite this delay, all atrial impulses do eventually reach the ventricles, maintaining a 1:1 ratio between P waves and QRS complexes. First-degree block can occur in otherwise healthy individuals or may indicate underlying cardiac issues, making it an important finding in EKG interpretation.

Characteristics of First-Degree Block
- Rhythm: Regular
- Rate: Usually normal (60–100 bpm), but depends on the underlying rhythm
- P wave: Present and normal in appearance, one P wave for each QRS complex
- PR interval: Prolonged (>0.20 secs), consistent delay from beat to beat
- QRS complex: Normal duration (<0.12 secs) and morphology
- Tolerance: Generally well-tolerated, usually asymptomatic. It may precede other forms of blocks
Clinical Significance
- Often a benign finding, especially in young, healthy individuals
- May be the first sign of more advanced conduction system disease
- First-degree AV block can be transient or permanent
Signs & Symptoms
- Typically asymptomatic
- Rarely may cause mild exercise intolerance
Treatment
- Usually no specific treatment needed
- Address underlying causes if identified
- Regular follow-up to monitor for progression to higher-degree blocks
Causes
- Normal variant in athletes or young adults
- Age-related degenerative changes
- Certain medications (e.g., beta-blockers, calcium channel blockers, digoxin)
- Elevated cardiac vagal tone
- Ischemic heart disease
- Electrolyte imbalances (e.g., hyperkalemia)
- Inflammatory conditions (e.g., myocarditis, Lyme carditis)
2. Second-Degree Block Type I (Wenckebach or Mobitz I)
Wenckebach phenomenon, also known as Mobitz Type I second-degree AV block, is an intriguing cardiac conduction abnormality. In this condition, there is a progressive delay in the AV conduction with each heartbeat until an atrial impulse fails to conduct to the ventricles completely. This results in a characteristic pattern on the EKG where the PR interval gradually lengthens until a P wave is not followed by a QRS complex, creating a “dropped” beat. After the dropped beat, the cycle repeats, often with a shorter initial PR interval.
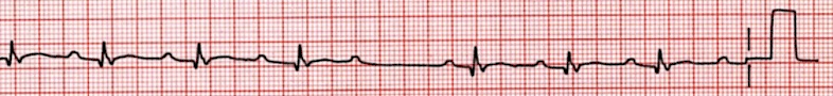
Characteristics of Second-Degree Type I Block (Wenckebach)
- Rhythm: Irregular due to periodic dropped beats
- Rate: Atrial rate normal (60–100 bpm), ventricular rate slightly lower due to dropped beats
- P wave: Present and consistent morphology
- PR interval: Progressively elongates until dropped beat, shortest PR interval after dropped beat
- QRS complex: Usually normal in duration and morphology, periodically absent (i.e., dropped beat)
- Tolerance: Generally well-tolerated, may cause mild symptoms
Clinical Significance
- Often benign, especially if occurring during sleep or in well-trained athletes
- May indicate underlying conduction system disease or cardiac ischemia
- Can progress to higher-degree AV blocks in some cases
Signs & Symptoms
- Often asymptomatic
- Some patients may experience symptoms of bradycardia and decreased cardiac output, such as dizziness or lightheadedness, fatigue, or palpitations
Treatment
- Usually no specific treatment required if asymptomatic
- Address underlying cause if identified
- In symptomatic cases: atropine for acute management, consider permanent pacemaker if consistent and asymptomatic
Causes
- Elevated cardiac vagal tone (e.g., in athletes or during sleep)
- Acute inferior myocardial infarction
- Certain medications (e.g., beta-blockers, calcium channel blockers, digoxin)
- Degenerative conduction system disease
- Electrolyte imbalances
- Inflammatory conditions (e.g., myocarditis, Lyme carditis)
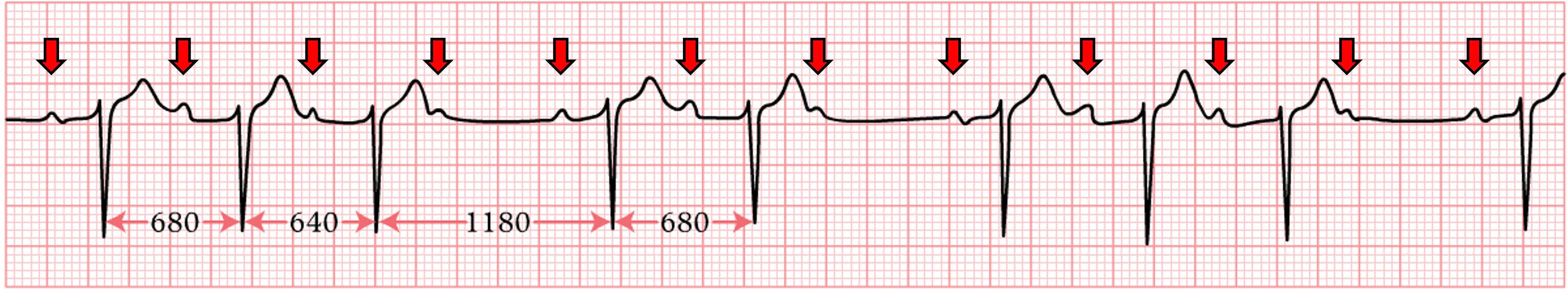
3. Second-Degree Block Type II (Mobitz II)
Mobitz Type II second-degree AV block is a more serious form of conduction disturbance than Type I. In this condition, some P waves are suddenly not conducted to the ventricles, resulting in “dropped” beats. Unlike Type I (Wenckebach), there is no progressive prolongation of the PR interval before the blocked beat. Mobitz II typically occurs below the AV node, often in the bundle of His or bundle branches, making it potentially more dangerous and less predictable than Mobitz I.
Characteristics of Second-Degree Type II Block
- Rhythm: Irregular due to intermittently dropped beats, no pattern to the dropped beats
- Rate: Atrial rate usually normal, ventricular rate lower due to non-conducted P waves
- P wave: Regular and consistent morphology, more P waves than QRS complexes
- PR interval: Constant in conducted beats, no progressive prolongation before dropped beats
- QRS complex: Often wide (>0.12 secs) due to location of block
- Tolerance: Frequently results in more severe symptoms of hemodynamic instability compared to second-degree type I. Greater risk of deteriorating into third-degree heart block.
Clinical Significance
- More serious than Wenckebach, often indicating significant conduction system disease
- Higher risk of progressing to a complete AV block
- May require immediate intervention, especially if symptomatic
Signs & Symptoms
- Can be asymptomatic in some cases
- Common symptoms include dizziness or syncope, fatigue, shortness of breath, or chest discomfort
Treatment
- Close monitoring and evaluation for all patients
- Temporary pacing may be required in emergency or urgent settings
- Permanent pacemaker implantation often recommended, especially if symptomatic
- Address underlying conditions if identified
Causes
- Chronic degenerative conduction system disease
- Acute myocardial infarction, especially anterior wall infarctions
- Fibrosis of the cardiac conduction system
- Infiltrative cardiac diseases (e.g., sarcoidosis, amyloidosis)
- Rarely, electrolyte imbalances or acute inflammatory conditions
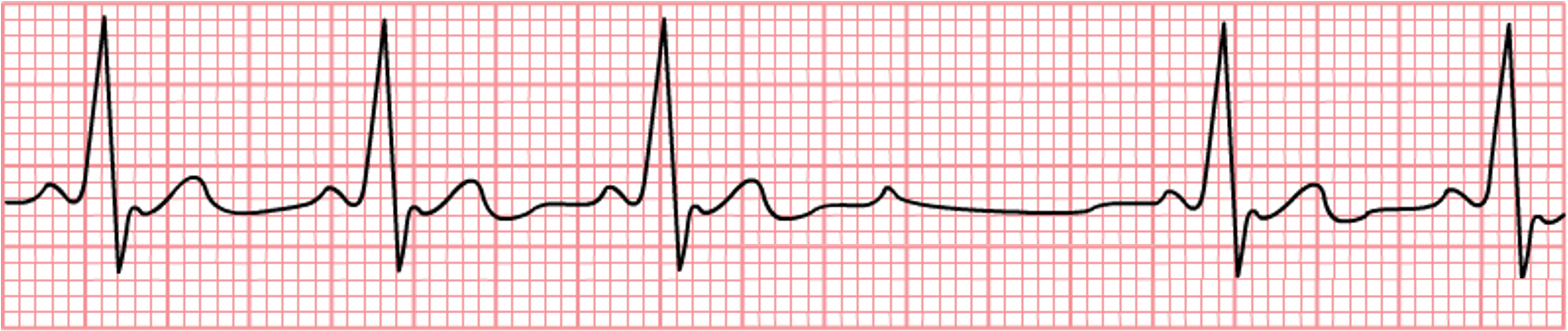
4. Third-Degree Block
In the most severe form of AV conduction disturbance, the electrical impulses between the atria and ventricles are completely dissociated. This condition, known as third-degree AV block or complete heart block, results in the atria and ventricles beating independently of each other. The ventricles rely on an escape rhythm originating from the AV junction or the ventricles themselves, while the atria continue to be paced by the SA node. This profound disruption in cardiac conduction can lead to significant hemodynamic compromise and necessitates prompt recognition and management.
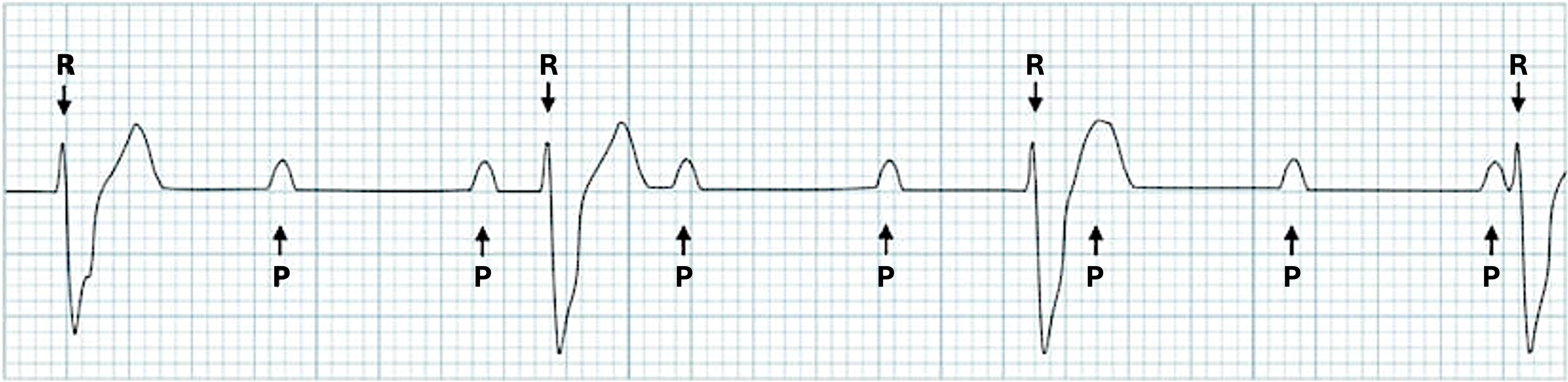
Characteristics of Third-Degree Block
- Rhythm: Atrial rhythm usually regular, ventricular rhythm usually regular but slower. No relationship between P waves and QRS complexes
- Rate: Atrial rate normal (60–100 bpm), ventricular rate typically slow (≤20–40 bpm)
- P wave: Present and regular, completely disjointed from QRS complexes
- PR interval: Not measurable due to AV dissociation, P waves and QRS complexes occur independently
- QRS complex: Regular, wide (>0.12 secs) if originating from ventricles (ventricular escape rhythm), may be narrow if originating from AV junction (junctional escape rhythm)
- Tolerance: Poorly tolerated, especially if ventricular rate is extremely slow. High risk of hemodynamic instability and syncope.
Clinical Significance
- Serious and potentially life-threatening arrhythmia
- Requires immediate medical attention and often permanent pacemaker implantation
- Can lead to sudden cardiac death if untreated
Signs & Symptoms
- Syncope or near-syncope
- Severe dizziness or lightheadedness
- Fatigue and weakness
- Palpitations
- Shortness of breath
- Chest pain or discomfort
Treatment
- Immediate temporary pacing in symptomatic or unstable patients
- Atropine may be used as a temporary measure to increase heart rate
- Permanent pacemaker implantation is usually necessary
- Treat underling causes if identified
Causes
- Degenerative conduction system disease (most common in older adults)
- Acute myocardial infarction, especially involving the AV node
- Infiltrative cardiac diseases (e.g., sarcoidosis, amyloidosis)
- Severe electrolyte imbalances
- Medications (e.g., digoxin toxicity, beta-blockers, calcium channel blockers)
- Congenital heart defects
- Post-cardiac surgery
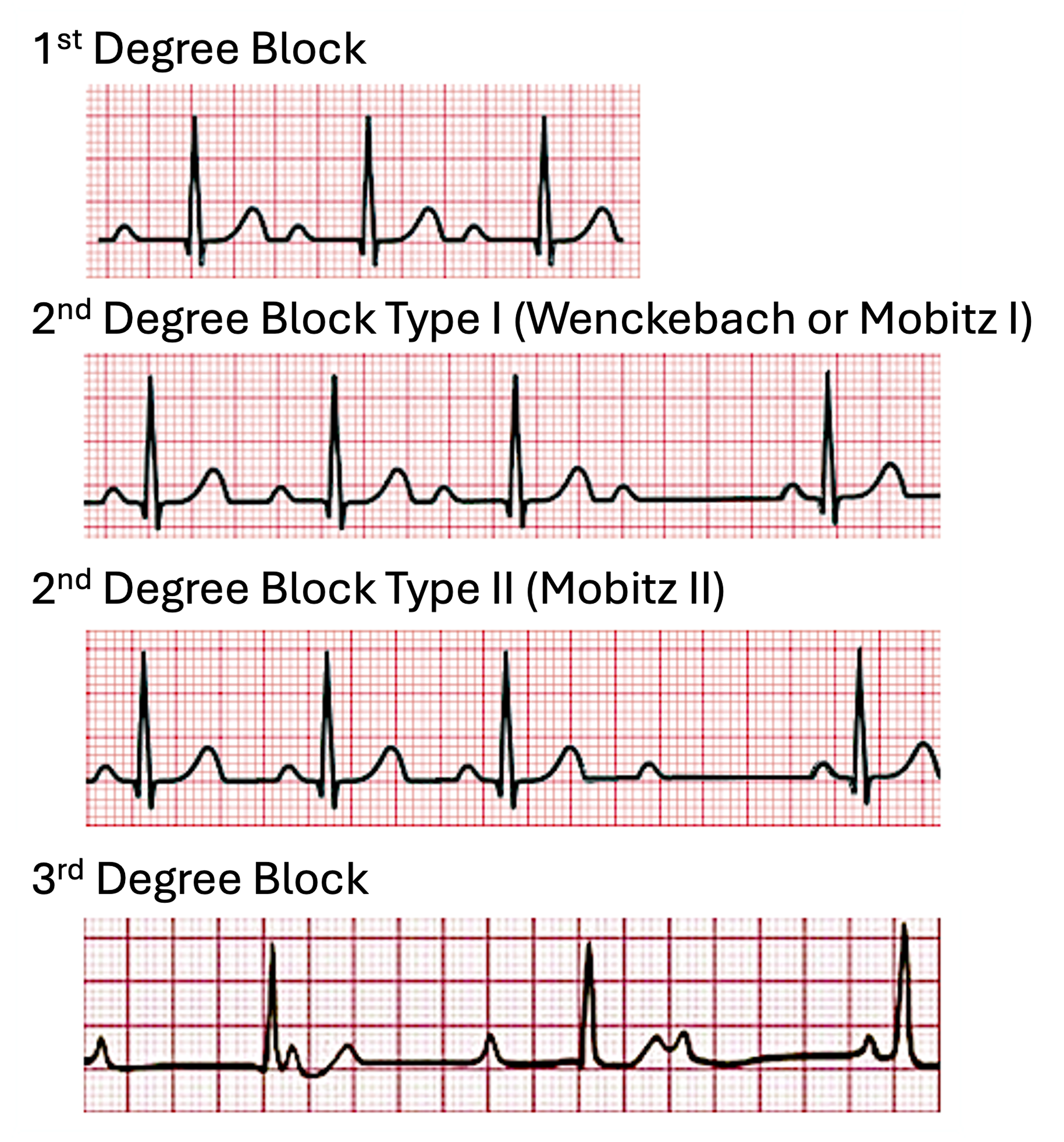
Image Attributions:
Fig. 8.1 – “Screenshot-2020-05-29-09.29.34.” by Simon Carley is licensed under CC BY-NC-SA 4.0 / Cropped from original
Fig. 8.2 – “Screenshot-2020-05-29-09.31.48.” by Simon Carley is licensed under CC BY-NC-SA 4.0 / Cropped from original
Fig. 8.3 – “Wenckebach2” by CardioNetworks is licensed under CC BY-NC-SA 4.0 / Cropped from original, added red arrows
Fig. 8.4 – “De-Rhythm Mobitz (CardioNetworks ECGpedia)” by CardioNetworks is licensed under CC BY-NC-SA 4.0 / Removed title
Fig. 8.5 – “Third degree heart block” by John Larkin and Robert Buttner is licensed under CC BY-NC-SA 4.0 / added more “P” and “R” labels
Fig. 8.6 – “Heart block” by Nicholas Patchett is licensed under CC BY-SA 4.0 / Edited rhythm titles and removed “Second degree AV block (2:1 block)”