5 Atrial Arrhythmias
Mechanisms and Types of Atrial Arrhythmias
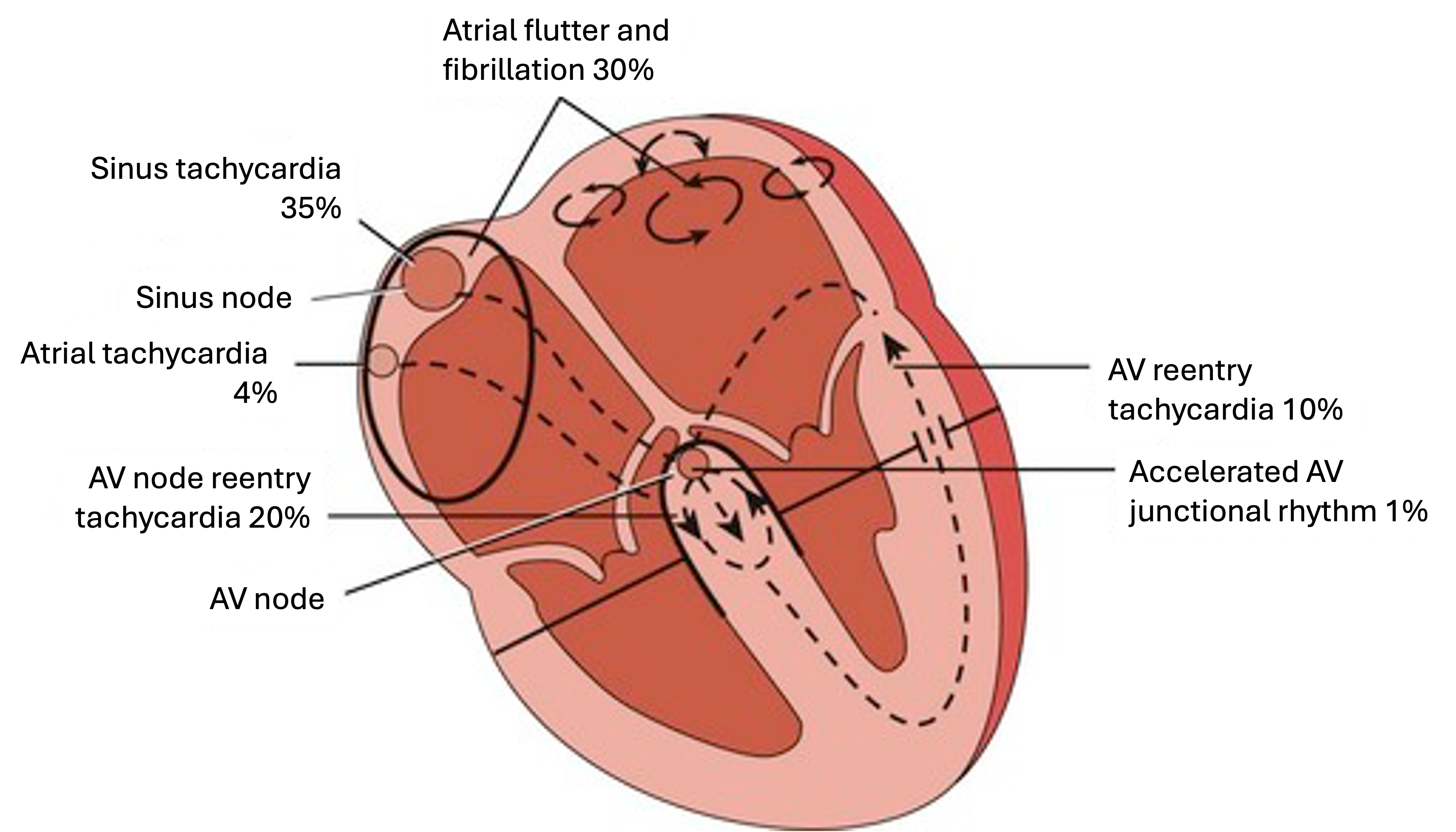
Atrial arrhythmias are abnormal heart rhythms that originate in the atria. These arrhythmias occur when the normal rhythm is disrupted by premature or irregular electrical impulses originating from the atrial tissue. Atrial arrhythmias can vary in severity, from benign conditions to serious disorders that may require medical intervention. The three main mechanisms behind the onset of atrial arrhythmias include altered automaticity, reentry, and afterdepolarizations.
Altered Automaticity
- Automaticity refers to the ability of cardiac cells to spontaneously generate electrical impulses. In the heart, the SA node is the primary pacemaker, but other regions like the AV node and Purkinje fibers also exhibit automaticity.
- Increased automaticity in the atria can lead to atrial tachyarrhythmias, such as:
- Atrial tachycardia: rapid firing from an ectopic atrial focus
- Multifocal atrial tachycardia: several atrial foci firing irregularly
Reentry
- Reentry is a mechanism where the electrical impulse travels in a circular or re-entrant pathway, thus perpetuating the impulse. For reentry to occur, there must be a region of unidirectional blocked and slow conduction, allowing the impulse to re-excite myocardial tissue it has already innervated.
- Atrial arrhythmias caused by reentry include:
- Atrial flutter: a rapid, organized atrial rhythm with a re-entrant circuit
- Atrial fibrillation: multiple, chaotic re-entrant electrical impulses in the atria
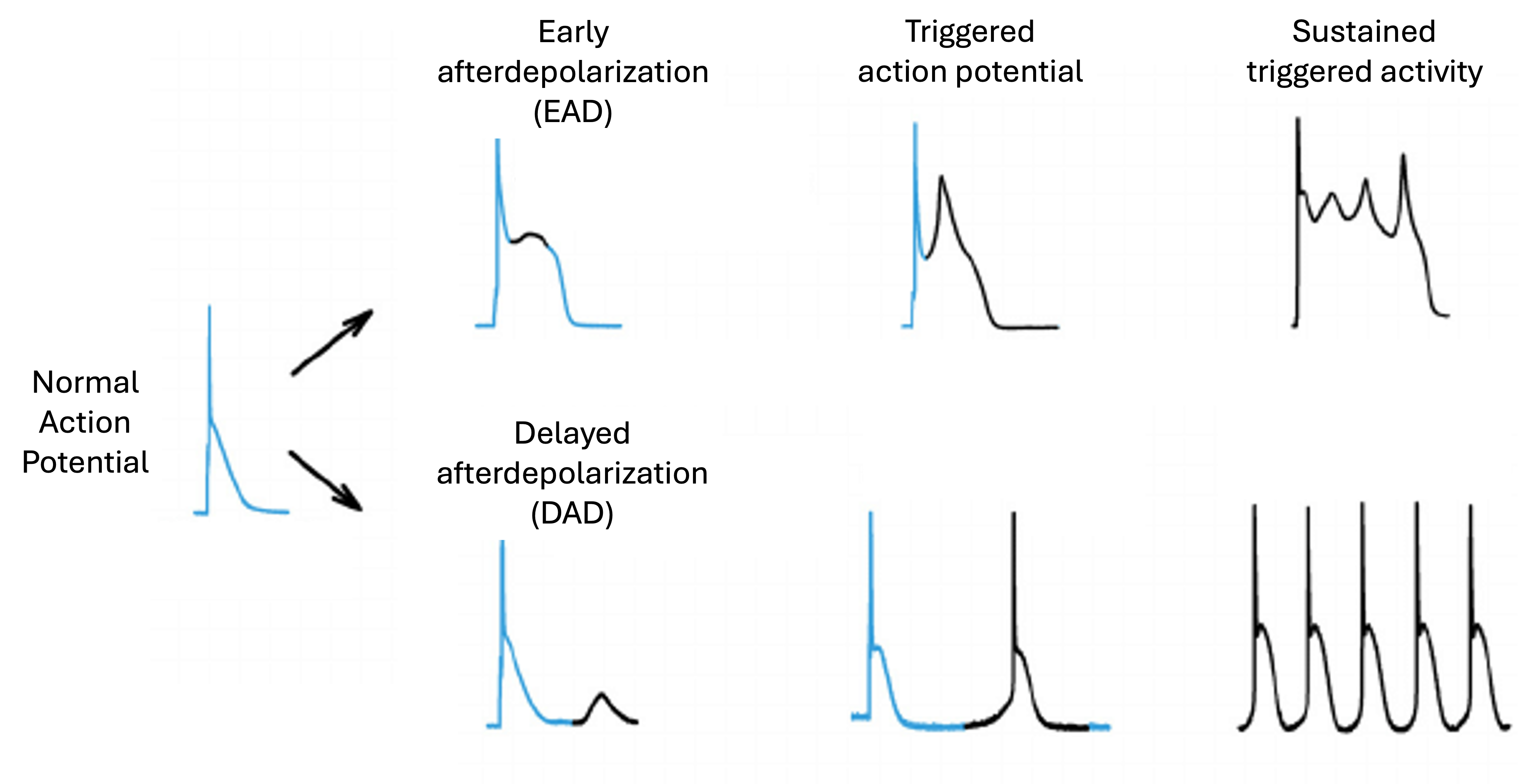
Afterdepolarizations
- Afterdepolarizations are abnormal depolarizations that occur after the completion of the normal action potential. They can be classified as:
- Early afterdepolarizations (EADs): occur during the plateau or repolarization phase of the action potential
- Delayed afterdepolarizations (DADs): occur after complete repolarization, during diastole
- If an afterdepolarization reaches the threshold potential, it can trigger an extra impulse, leading to atrial arrhythmias including atrial tachycardia, atrial fibrillation, or ectopic beats.
1. Premature Atrial Contractions
A premature atrial contraction (PAC) is an early, extra beat originating from the atria before the next expected normal sinus beat. Below are key points regarding PACs:
- Caused by an abnormal electrical impulse firing prematurely from somewhere within the atria, outside of the normal SA node
- PACs can feel like a fluttering, skipped beat, or extra beat sensation in the chest
- Generally, PACs are considered benign when infrequent, but frequent PACs may increase the risk of developing atrial fibrillation or indicate an underlying heart disorder
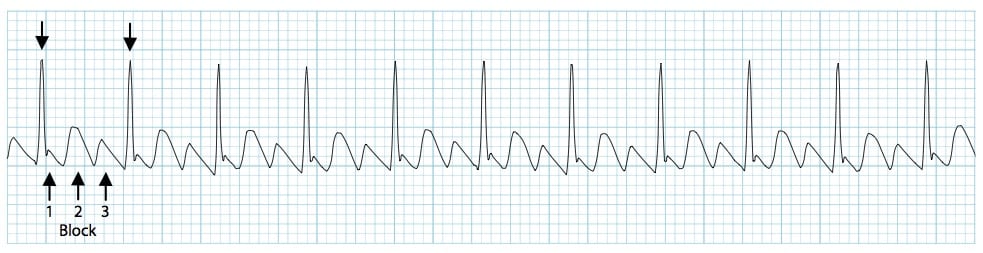
Premature atrial contractions can manifest in various forms on the EKG, depending on the origin and timing of the ectopic impulse:
- If the ectopic focus is located near the SA node, the premature P wave may precede the QRS complex but exhibit a different morphology compared to a normal sinus P wave
- In certain cases, the premature P wave can become superimposed on the preceding T wave, altering the T wave’s appearance
- When an early atrial impulse fails to conduct through the AV node to the ventricles, it results in a blocked PAC. This is seen as an isolated P wave without a subsequent QRS complex on the EKG
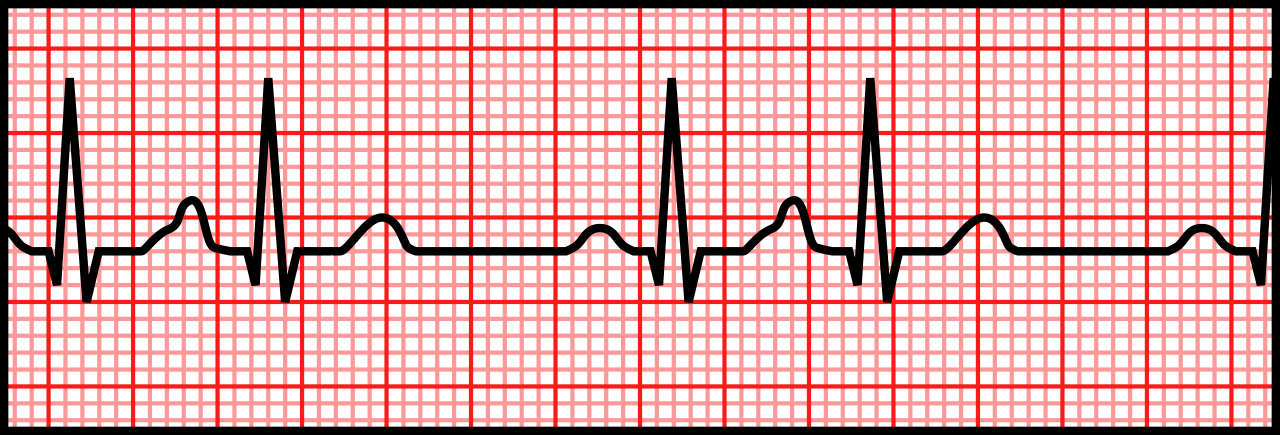
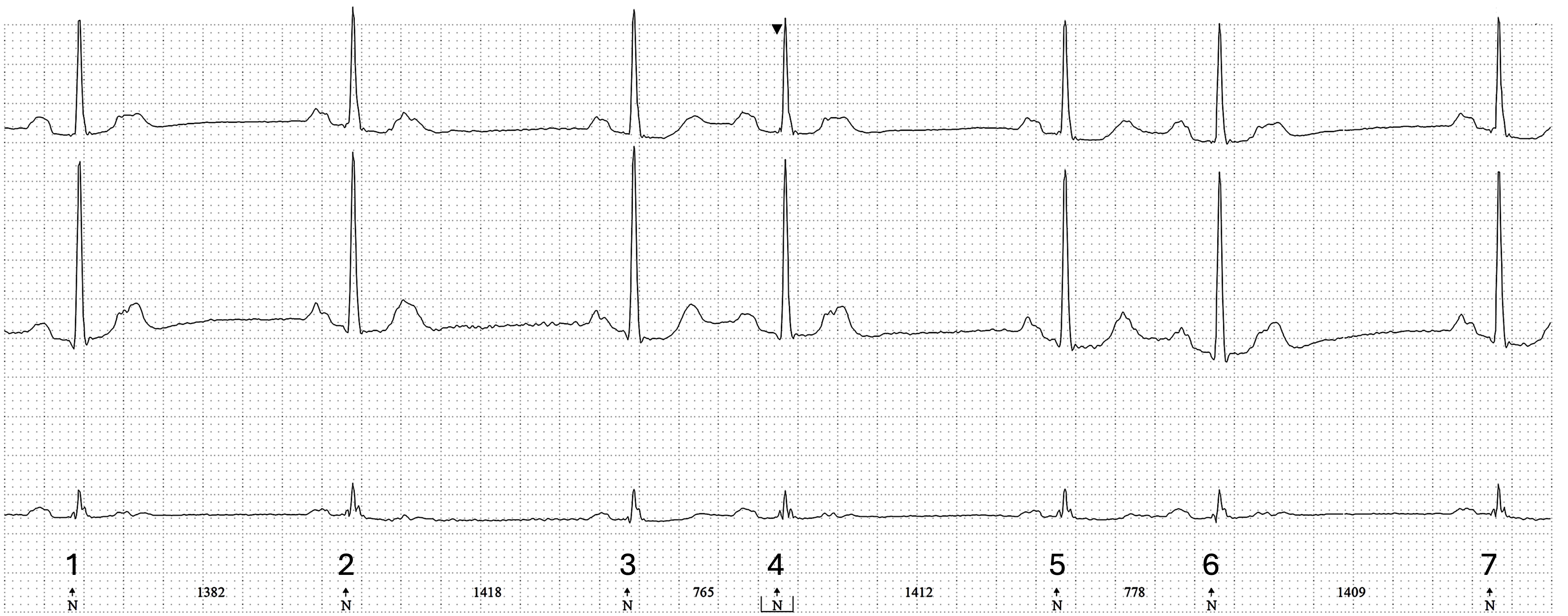
In Figure 5.4, the EKG shows a complex rhythm featuring sinus bradycardia (approx. 40 bpm) with frequent PACs. The first, fifth, and last QRS complexes are sinus beats, spaced approximately 1400 ms apart. Small deflections can be seen on the T waves of the first and second QRS, which is not visible after the third QRS, especially in the middle and lower leads. These are very closely coupled PACs that were not conducted through the AV node since the ventricles are still in the refractory period. The fourth and sixth QRS complexes are likely conducted PACs, that are both followed by a blocked PAC.
Characteristics of PACs
- Rhythm: Irregular due to the pause following the PAC. This pause is typically not long enough to fully compensate for the prematurity of the ectopic beat, resulting in an incomplete resetting of the sinus node rhythm.
- Rate: Depends on the underlying rhythm
- P wave: Premature, abnormal, and different from the SA node P wave
- PR interval: Normal, prolonged, or short
Tolerance
- Most patients sustain normal cardiac output despite experiencing PACs. However, PACs can occasionally trigger short episodes of rapid atrial tachycardia.
- When this happens, patients might exhibit symptoms such as palpitations, skipped/fluttering beats, dizziness, chest discomfort, shortness of breath, or anxiety when having more frequent PAC episodes.
- Most people with occasional, infrequent PACs are asymptomatic and tolerate them well without any treatment needed, as they are generally considered a benign phenomenon in otherwise healthy individuals.
Treatment
- In many instances, no specific treatment is necessary if PACs occur infrequently and the patient is asymptomatic.
- Lifestyle changes, such as reducing caffeine and alcohol intake and managing stress may help lower the frequency of PACs.
- Anti-arrhythmic medications (e.g., beta-blockers, calcium channel blockers) can be used to manage frequent or symptomatic PACs.
- Catheter ablation may be an option for patients who do not respond to medication and have significant symptoms, or if PACs increase the risk of atrial fibrillation.
Causes
- May be associated with underlying heart conditions such as coronary artery disease, heart failure, cardiomyopathy, and valvular heart disease.
- Can be triggered by factors like stress, anxiety, caffeine, alcohol, smoking, dehydration, and electrolyte imbalances.
- Certain medications like decongestants or bronchodilators can increase PAC frequency.
- Often the exact cause is unknown or idiopathic, especially in otherwise healthy individuals.
2. Atrial Tachycardia
Atrial tachycardia is a type of supraventricular tachycardia (SVT), indicating that the impulse causing the rapid heart rate originates from a location above the ventricles. It occurs when an ectopic atrial impulse rapidly and repeatedly cycles to and from the ventricles through a circular pathway in the AV node. When there are three or more consecutive atrial ectopic beats, it is classified as atrial tachycardia. This condition can be triggered by a PAC. It can lead to a shortened diastole, reduced atrial kick, decreased cardiac output, and diminished coronary perfusion.

Characteristics of Atrial Tachycardia
- Rhythm: Regular
- Rate: Ventricular rate is typically identical to the atrial rate
- P wave: Abnormal – often difficult to recognize
- PR interval: Usually obscured and unmeasurable
- QRS complex: Typically normal but can appear wide if there is abnormal conduction
- Tolerance: Some patients may remain asymptomatic, while others experience significant discomfort and symptoms. Long-term tolerance may be influenced by underlying heart conditions or the presence of other comorbidities.
Clinical Significance
- Often benign in otherwise healthy individuals, but can lead to cardiomyopathy and heart failure if persistent or unceasing.
- May increase the risk of developing more serious arrhythmias like atrial fibrillation over time.
- Underlying heart disease or other conditions may be present, requiring evaluation and management.
Signs & Symptoms
- While some patients may maintain normal cardiac output, others may present palpitations, lightheadedness, dizziness, syncope, dyspnea, chest pain or discomfort, or fatigue.
Treatment
- Vagal maneuvers, such as the Valsalva maneuver or carotid sinus massage.
- Antiarrhythmic medications like beta-blockers, calcium channel blockers to control rate and rhythm.
- Treatment of any underlying conditions like heart disease, thyroid disorders, or electrolyte imbalances.
- Catheter ablation to destroy the abnormal electrical focus or circuit.
- Cardioversion (electrical or chemical) for acute rate control.
Causes
- Idiopathic or unknown cause, especially in younger individuals.
- Structural heart disease like cardiomyopathy, previous MI, and valvular disorders.
- Electrolyte disturbances, thyroid disorders, excessive alcohol or caffeine use.
- Certain medications like decongestants, bronchodilators, and stimulants.
- Pregnancy, recent heart surgery, infections.
3. Multifocal Atrial Tachycardia
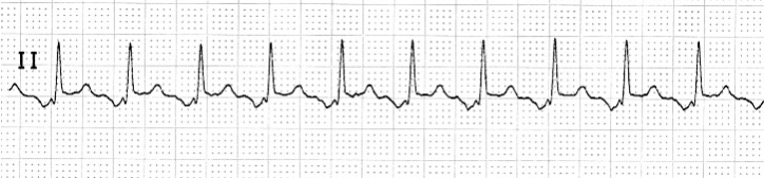
Characterized by multiple atrial foci firing irregularly, multifocal atrial tachycardia (MAT) is an SVT that results in an irregular atrial rate and an irregular ventricular response. On an EKG, MAT is recognized by the presence of at least three different P wave morphologies, with varying PR intervals and irregular R-R intervals.
Characteristics of MAT
- Rhythm: Irregular rhythm with no discernible pattern
- Rate: Atrial rate is typically greater than 100 bpm
- P wave: At least three different P wave morphologies present
- PR interval: Variable due to the irregular conduction of atrial impulses
- QRS complex: Usually narrow unless there is an underlying conduction abnormality
- Tolerance: Often asymptomatic, but degree of tolerance can vary depending on the underlying condition
Clinical Significance
- Multifocal atrial tachycardia is relatively uncommon and frequently linked to various underlying conditions, including chronic obstructive pulmonary disease (COPD), coronary heart disease, congestive heart failure, electrolyte imbalances, diabetes, and chronic renal failure.
- The rapid and irregular atrial rate can potentially lead to decreased cardiac output and hemodynamic instability, particularly in patients with pre-existing heart conditions.
Signs & Symptoms
- Palpitations (sensation of a rapid, fluttering heartbeat)
- Shortness of breath, especially with exertion
- Chest discomfort or tightness
- Fatigue, weakness
- Some patients may not exhibit any symptoms, especially in early stages.
Treatment
- Treatment of underlying condition (e.g., pulmonary disorders, electrolyte imbalances).
- Rate control with medications such as beta-blockers, calcium channel blockers, digoxin.
- Antiarrhythmic drugs for rhythm control such as amiodarone and sotalol.
- Catheter ablation in refractory cases or if tachycardia-induced cardiomyopathy develops.
Causes
- COPD and other pulmonary disorders
- Electrolyte imbalances (e.g., hypokalemia, hypomagnesemia)
- Coronary artery disease
- Heart failure
- Renal failure
- Diabetes
- Postoperative infections such as sepsis
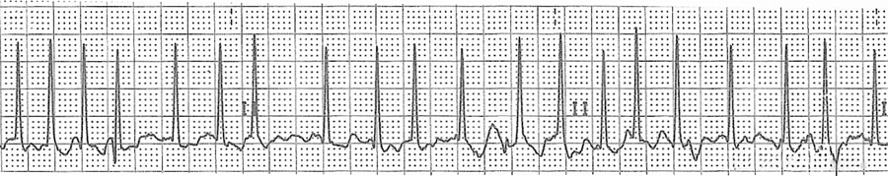
4. Atrial Flutter
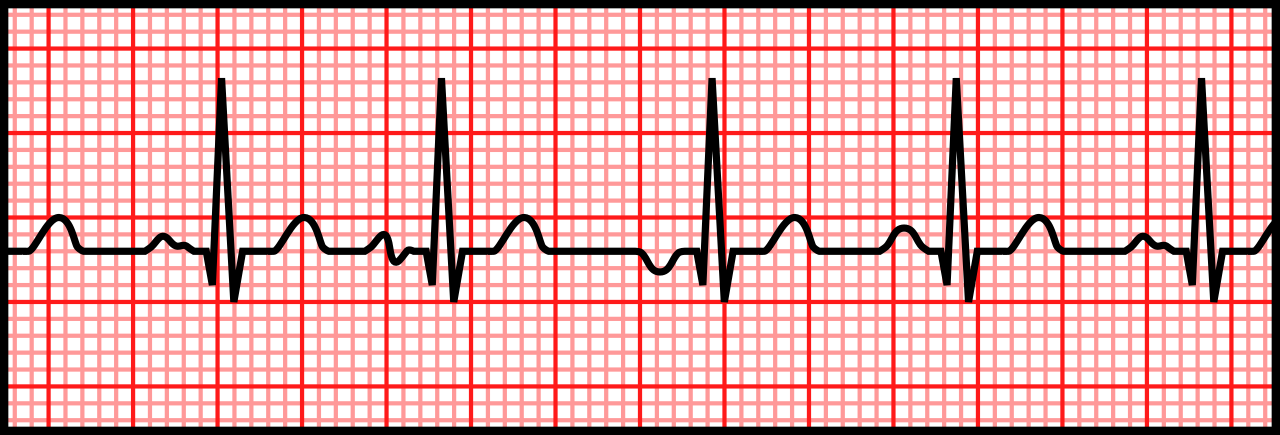
On an EKG, atrial flutter is recognized by the presence of saw-tooth-like flutter waves instead of distinct P waves. These flutter waves, or F waves, are a result of the continuous, circular propagation of electrical impulses within the atria.
Characteristics of Atrial Flutter
- Rhythm: Regular P-P interval. The R-R interval is usually regular, but can be irregular if the AV conduction rate varies
- Rate: Atrial rate typically between 250–350 bpm, ventricular varies
- P wave: Regular saw-tooth flutter (F) waves are present before each QRS complex, can be two, three, four, or more F waves (2:1, 3:1, 4:1)
- PR interval: Usually obscured and unmeasurable, not necessary to measure
- QRS complex: Usually normal
- Tolerance: Some patients may maintain adequate cardiac output while others may be symptomatic
Clinical Significance
- Atrial flutter is a type of supraventricular tachycardia that, if left untreated, can lead to serious complications such as stroke, heart failure, and inadequate cardiac output. There is a heightened risk of the rhythm progressing to atrial fibrillation, which further amplifies the risk of complications.
Signs & Symptoms
- Palpitations (sensation of a rapid, fluttering heartbeat)
- Shortness of breath, fatigue, or exercise intolerance
- Chest discomfort or tightness
- Lightheadedness or dizziness
- Some patients may not exhibit any symptoms.
Treatment
- Rate control with medications such as beta-blockers, calcium channel blockers, or digoxin.
- Rhythm control with antiarrhythmic drugs like amiodarone or sotalol.
- Electrical cardioversion to restore sinus rhythm.
- Catheter ablation targeting the atrial flutter circuit.
Causes
- Underlying heart conditions such as coronary heart disease, valvular heart disease, or cardiomyopathy.
- Acute MI, congenital heart defects, hypertension
- COPD
- Previous heart surgery or ablation procedures
- Thyroid disorders, particularly hyperthyroidism
- Excessive alcohol consumption
- Electrolyte imbalance
- Certain medications or stimulants.
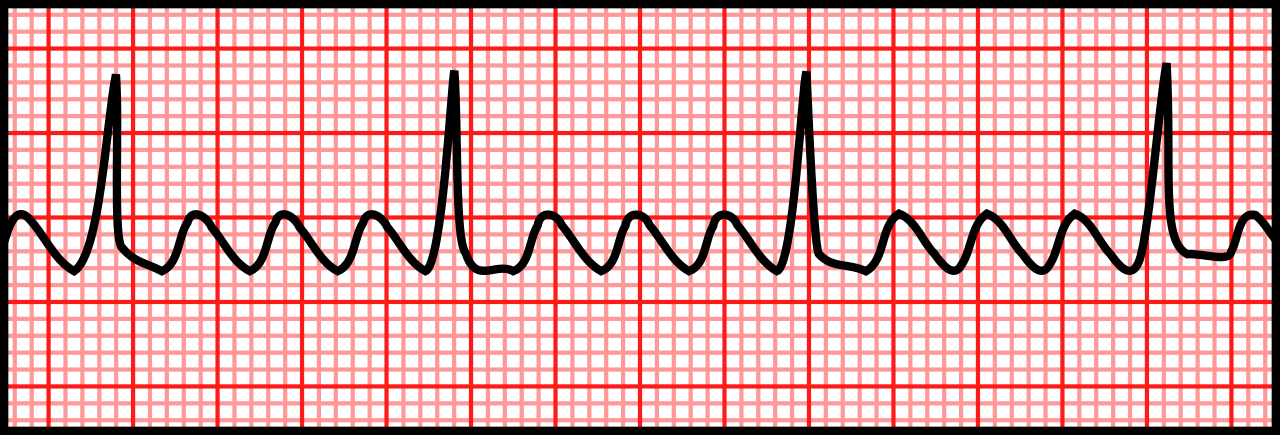
5. Atrial Fibrillation
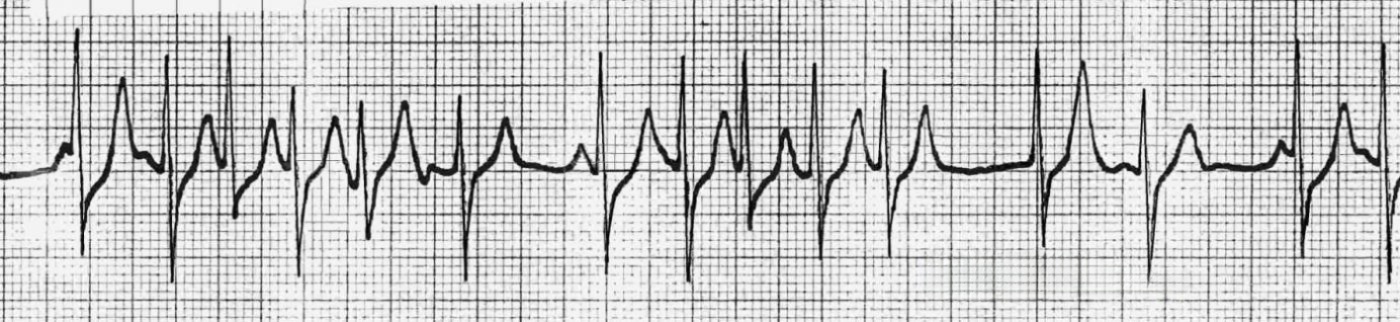
Characterized by chaotic and disorganized electrical activity in the atria, atrial fibrillation (A-fib) leads to ineffective atrial contractions. On an EKG, A-fib is identified by the absence of distinct P waves, which are replaced by irregular fibrillatory waves or an irregular isoelectric baseline. The three main types of A-fib are paroxysmal (intermittent, self-terminating episodes), persistent (sustained episodes requiring intervention), and long-standing persistent (continuous A-fib over 12 months, often with structural atrial remodeling).
Listen to Atrial Fibrillation
Characteristics of Atrial Fibrillation
- Rhythm: Irregularly irregular
- Rate: Atrial rate is 350 bpm or greater, is unmeasurable
- P wave: Absent
- PR interval: Not measurable
- QRS complex: Normal
- Tolerance: Most patients can tolerate A-fib if rate is controlled and remains below 100 bpm. However, those with uncontrolled A-fib, where the rate exceeds 100 bpm or drops below 60 bpm, may experience symptoms
Clinical Significance
- The most common sustained cardiac arrhythmia, affecting millions of people worldwide.
- Atrial fibrillation increases risk of stroke, heart failure, and other cardiovascular complications.
Signs & Symptoms
- Palpitations, irregular heartbeat
- Shortness of breath, fatigue
- Chest discomfort or tightness
- Lightheadedness or dizziness
- Some patients, particularly those with paroxysmal A-fib, may not exhibit symptoms.
Treatment
- Rate control with medication such as beta-blockers, calcium channel blockers, or digoxin.
- Rhythm control with antiarrhythmic drugs such as amiodarone, sotalol, or dofetilide.
- Anticoagulation therapy to lower stroke risk.
- Electrical cardioversion to restore sinus rhythm.
- Catheter ablation targeting pulmonary vein isolation or other strategies.
Causes
- Underlying heart conditions such as coronary heart disease, valvular heart disease, or cardiomyopathy.
- Hypertension, diabetes, obesity, and other metabolic disorders
- Excessive alcohol consumption or stimulant use
- Anemia
- Thyroid disorders, particularly hyperthyroidism
- Congenital heart defects
- Aging and genetic factors
Image Attributions: