4 Sinus Node Arrhythmias
Sinus node arrhythmias are abnormal cardiac rhythms originating from the sinoatrial (SA) node, the primary pacemaker of the heart. These arrhythmias can occur when the SA node either generates impulses at irregular intervals or fails to initiate an impulse. They can range from benign conditions to more serious disorders requiring medical attention.
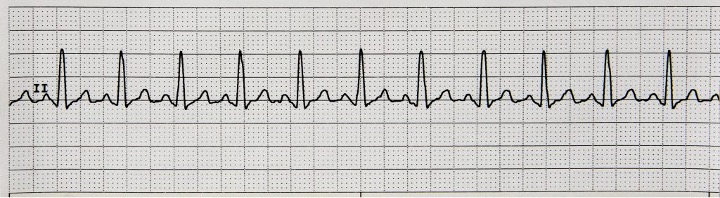
1. Sinus Tachycardia
Characteristics of Sinus Tachycardia
- Origin: SA node
- Rhythm: Regular
- Rate: 100 – 180 bpm
- P wave: Precede each QRS with normal deflection in each lead
- PR interval: Normal but shortens in relation to the PR interval found in NSR
- QRS width: Normal
- Mechanism: Physiologically enhanced automaticity
- Tolerance: Generally well-tolerated, but may cause palpitations or shortness of breath
- Typically has a gradual onset and decline, reflecting the body’s natural response to various stimuli or the progression of underlying conditions
Clinical Significance
- The significance of sinus tachycardia depends on its underlying cause, which can include exercise, emotional stress, hypovolemia, hemorrhage, or pain.
- While often physiological, persistent or unexplained, sinus tachycardia may not be benign and can indicate underlying health issues.
- Unexplained sinus tachycardia can weaken the heart over time, potentially leading to tachycardia-induced cardiomyopathy if not addressed. It might also signal poor prognosis, indicating underlying conditions requiring attention.
- May lead to angina in cardiac patients due to increased myocardial oxygen demands.
- After acute myocardial infarction (MI), the presence of sinus tachycardia can be a sign of massive cardiac damage, imminent heart failure, or cardiogenic shock, resulting in poorer prognosis.
Signs & Symptoms
- Usually asymptomatic except for a rapid pulse.
- If cardiac output declines, patient may experience angina, hypotension, syncope, and blurred vision. The patient may also report a pounding sensation in chest and feelings of nervousness.
Treatment
- Treatment is not necessary unless the patient is symptomatic.
- May need to decrease caffeine intake, tobacco use, alcohol use, or certain over-the-counter drug intake (e.g., cold medicines can cause increases in heart rate).
- If sinus tachycardia leads to ischemia, drugs used to slow heart rate (i.e., lower myocardial oxygen demand) may include:
- Beta-adrenergic blockers: metoprolol (Lopressor), atenolol (Tenormin), nadolol (Corgard)
- Calcium channel blockers: verapamil (Verelan)
Causes
- Sinus tachycardia is a normal response to exercise, pain, anxiety, stress, fever, and fear.
- Can also present in heart failure, cardiogenic shock, and pericarditis.
- It acts as a compensatory mechanism in conditions like anemia, shock, pulmonary embolism, and respiratory distress.
- Can also occur due to certain drug intake such as:
- atropine, epinephrine, caffeine, dopamine, nicotine, cocaine, amphetamines, certain antidepressants, etc.
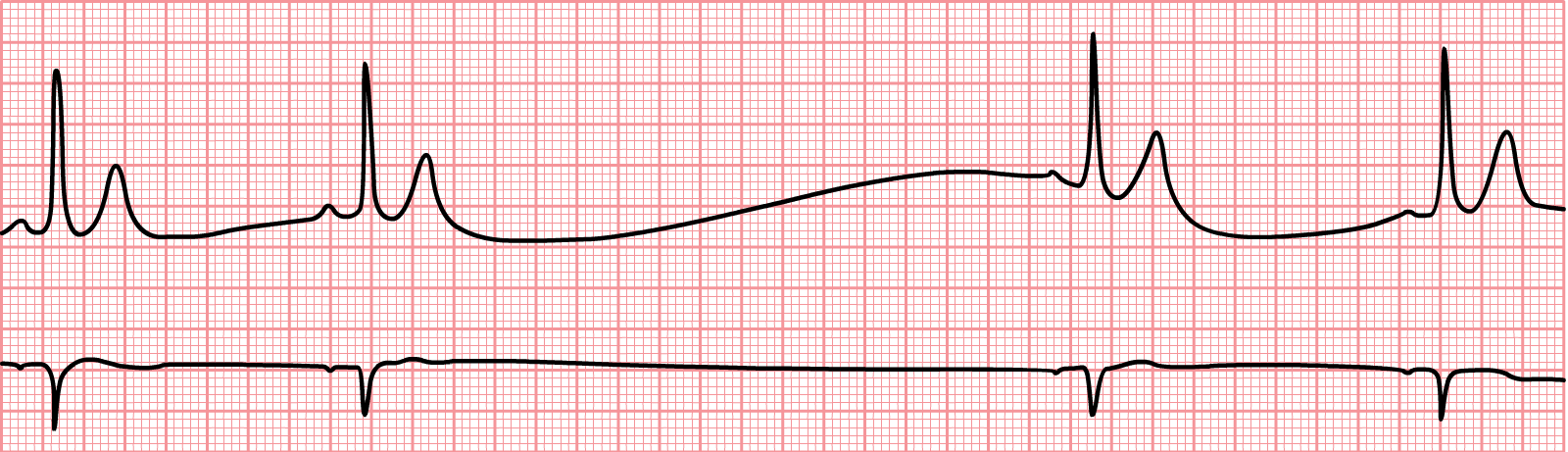
2. Sinus Bradycardia
Characteristics of Sinus Bradycardia
- Origin: SA node
- Rhythm: Regular
- Rate: Less than 60 bpm
- P wave: Precede each QRS complex with normal deflection in each lead
- PR interval: Normal but lengthens in relation to the PR interval found in NSR
- QRS width: Normal
- Mechanism: Enhanced vagal (parasympathetic) activity. Automaticity in SA node decreases
- Gradual onset and decline

Clinical Significance
- Sinus bradycardia is often a normal finding in healthy individuals, particularly young adults, athletes, or during sleep, and may not indicate pathology.
- However, symptomatic sinus bradycardia can lead to cerebral hypoperfusion, syncope, fatigue, and reduced exercise tolerance, impacting quality of life.
- Sinus bradycardia can be a marker of underlying cardiovascular disease, such as inferior wall MI or increased intracranial pressure, requiring prompt evaluation and management. It frequently occurs due to inferior MI involving the right coronary artery which supplies the SA node.
Signs & Symptoms
- Cool, clammy skin, altered mental status, dizziness, blurred vision,
- Hypotension, cerebral hypoperfusion, and syncope
Treatment
- Observe patient; usually no treatment needed unless the patient is symptomatic.
- If symptomatic, review the patient’s medications, especially digoxin, beta-blockers, and calcium channel blockers, and consider any recent dosage increases.
- Sinus bradycardia in the context of hypothermia, hypoglycemia, or sleep apnea may require treatment of the underlying condition.
Causes
- Sinus bradycardia can arise from various non-cardiac and cardiac disorders:
- Non-cardiac conditions like hyperkalemia (i.e., elevated potassium levels)
- Situations that increase vagal tone or decrease sympathetic stimulation, such as sleep, the Valsalva maneuver, or vomiting, may precipitate sinus bradycardia.
- Cardiac diseases affecting the SA node, such as sick sinus syndrome or SA node dysfunction, are common causes of sinus bradycardia, especially in older adults.
- Myocardial ischemia or infarction, particularly acute inferior wall MI, can result in sinus bradycardia immediately after the event.
- Certain medications like digoxin, beta-blockers, calcium channel blockers, and others can induce or exacerbate sinus bradycardia as an adverse effect.
3. Sinus Arrhythmia
Characteristics of Sinus Arrhythmia
- Origin: SA node
- Rhythm: Irregular. The difference between the shortest and the longest P-P interval is >0.12 secs
- Rate: Slows with expiration and accelerates with inspiration. The slow phase may have rates less than 60 bpm
- P wave: Precede each QRS complex with identical or slight variation in morphology to sinus P waves
- PR interval: As sinus rate slows, PR interval lengthens
- QRS width: Normal
- Mechanism: Primarily mediated by cyclical changes in vagal tone during respiration, where inspiration decreases and expiration increases vagal effects on the SA node

Clinical Significance
- Sinus arrhythmia is more pronounced in children and athletes, and is generally considered a normal physiologic phenomenon and a sign of good cardiovascular health in these groups. However, in older adults, sinus arrhythmia might be a precursor to sick sinus syndrome.
- Non-respiratory sinus arrhythmia in adults, not associated with breathing, could signal underlying heart disease, autonomic neuropathy, or side effects of medications like digoxin.
- Cardiac output is typically unaffected.
Signs & Symptoms
- Respiratory sinus arrhythmia is often asymptomatic and an incidental finding.
- Although rare, non-respiratory sinus arrhythmia may cause dizziness, lightheadedness, and palpitations, especially if there is an underlying heart condition or overuse of certain medications.
Treatment
- Typically, no treatment is necessary for respiratory sinus arrhythmia, as it signifies heart health.
- Treatment for non-respiratory sinus arrhythmia focuses on addressing the underlying condition, which may involve adjusting medications, treating cardiovascular disease, and regular monitoring. Lifestyle changes and management of the root causes are also crucial.
Causes
- Respiratory sinus arrhythmia is primarily caused by the natural variation in heart rate that occurs with inhalation and exhalation.
- Potential causes of non-respiratory sinus arrhythmia include head or neck injuries, excessive use of medications such as digoxin, and underlying heart conditions such as heart disease or scarring of the sinus node.
4. Sinus Pause/Sinus Arrest
Sinus pause, also known as sinus arrest, is a cardiac arrhythmia characterized by a temporary interruption in the normal firing of the SA node. During a sinus pause, there is a brief cessation of electrical activity originating from the SA node, resulting in a pause in cardiac conduction system. This pause can last for a few seconds before the SA node resumes its function or a lower pacemaker site takes over. Sinus pauses can be a normal finding in some individuals, particularly during sleep, but prolonged or frequent pauses may indicate underlying issues and can lead to symptoms such as dizziness and syncope.
Characteristics of Sinus Pause/Sinus Arrest
- Rhythm: P-P and R-R intervals are constant except for the pause/arrest which is due to the absent PQRST
- Rate: Atrial and ventricular rates are within normal range except for the area the pause/arrest occurs
- PR interval: usually normal
- QRS width: usually normal
- SA node fails to generate an impulse
Clinical Significance
- Sinus arrest and sinus pause represent interruptions in the normal pacing of the heart, where the SA node temporarily fails to conduct an electrical impulse.
- Both conditions can lead to periods of bradycardia, which may decrease cardiac output and perfusion to vital organs.
- Frequent or severe sinus arrests or pauses can indicate an underlying heart condition and may progress to more serious arrhythmias, such as atrial fibrillation or ventricular tachycardia.
Signs & Symptoms
- Patients may feel palpitations or a sensation of skipped beats when the pause or arrest occurs.
- Reduced cardiac output during the pause can lead to dizziness or lightheadedness.
- In cases of prolonged pauses, patients may experience syncope due to cerebral hypoperfusion.
- Persistent bradycardia associated with frequent pauses can result in overall fatigue and weakness.
Treatment
- Stop medications that suppress SA node (e.g., digoxin, beta-blockers, calcium channel blockers). Intravenous atropine or isoproterenol can be used for temporary medical management while preparing for pacing.
- Permanent pacemaker implantation is the definitive treatment for symptomatic sinus arrest or frequent/prolonged sinus pauses.
- Reversible causes such as electrolyte disturbances, hypothyroidism, or medications (e.g., beta-blockers) that can exacerbate sinus node dysfunction should be addressed.
Causes
- The most common benign cause is increased vagal tone, especially in younger individuals under emotional stress or after Valsalva maneuvers.
- Certain medications such as beta-blockers, calcium channel blockers, digoxin, and antiarrhythmia drugs can depress sinus node function and promote pauses.
- Age-related degeneration or fibrosis of the SA node can impair its function, leading to potential pauses.
- Acute MI, particularly inferior wall infarction, can lead to sinus node ischemia and sinus arrest.
- Reversible causes like sleep apnea, hypothyroidism, increased intracranial pressure, and autonomic neuropathies can also contribute to sinus pauses.
5. Sick Sinus Syndrome
Sick sinus syndrome is a group of heart rhythm disorders caused by dysfunction of the SA node. This condition can result in bradycardia, pauses in the heart’s electrical activity, or alternating periods of slow and fast heart rhythms (i.e., bradycardia-tachycardia syndrome). Sick sinus syndrome is more common in older adults.
Here are some further details on sick sinus syndrome:
- Can lead to bradyarrhythmias (e.g., sinus bradycardia, sinus pauses/arrest), tachyarrhythmias (e.g., atrial fibrillation), or alternating brady-tachycardia. Increases risk of complications like heart failure, stroke, and sudden death.
- Often asymptomatic initially. Depending on the type of arrhythmia present, sick sinus syndrome can cause palpitations, dizziness, syncope, fatigue, dyspnea, or angina.
- Risk factors for sick sinus syndrome include age, heart disease, prior heart surgery, and medications affecting SA node function.
- Pacemaker implantation is the definitive treatment for symptomatic bradyarrhythmias. Dual-chamber pacemakers preferred. Antiarrhythmic drugs may be added for tachyarrhythmias. Reversible causes like electrolyte disturbances should be corrected.
- Usually inappropriate response to exercise, heart rate fails to increase.
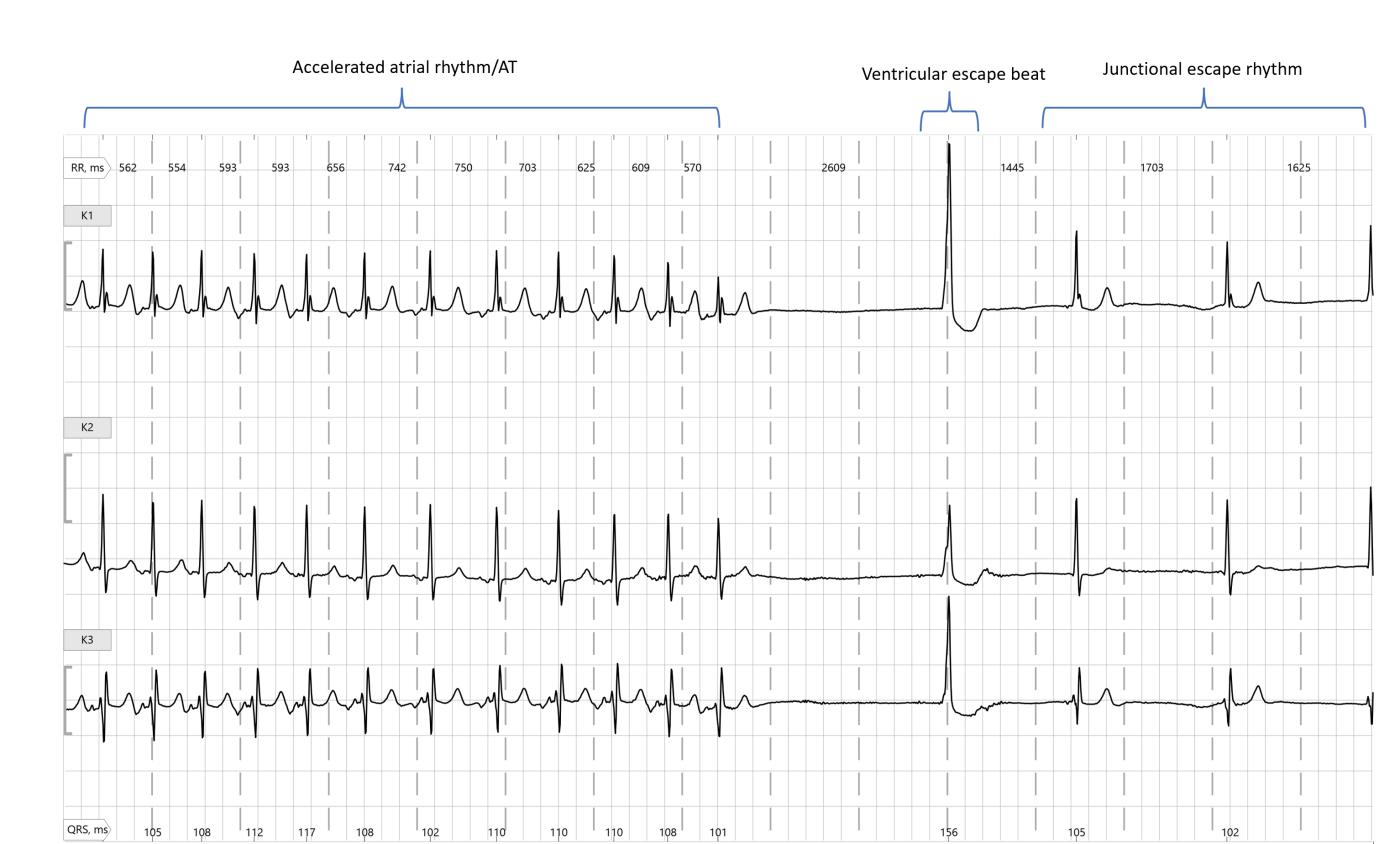
Image Attributions:
Fig 4.1 – “Sinus Tachycardia” by Deanna Hoyord is licensed under CC BY 4.0
Fig. 4.2 – “Sinus Bradycardia” by Deanna Hoyord is licensed under CC BY 4.0
Fig. 4.3 – “ECG Sinus Arrhythmia 79 bpm” by Scott Ewing is licensed under CC BY 4.0 / cropped from original and grayscaled
Fig. 4.4 – “Sinusarrest” by CardioNetworks is licensed under CC BY-NC-SA 4.0
Fig. 4.5 – “Escape” by Dr. A Röschl is licensed under CC BY-NC-SA 4.0
Beta-blockers are medications that reduce the effects of adrenaline on the heart and blood vessels, commonly used to treat cardiovascular conditions such as high blood pressure, angina, and arrhythmias, as well as other conditions like migraines and anxiety.
Medications that inhibit the influx of calcium ions into cardiac and smooth muscle cells, primarily used to treat hypertension, angina, and certain arrhythmias by promoting vasodilation and reducing heart rate and contractility.
A medication used to treat heart conditions, particularly congestive heart failure and atrial fibrillation, by increasing the strength of heart contractions and regulating heart rate.
An anticholinergic medication that blocks the effects of acetylcholine at muscarinic receptors, used primarily to treat bradycardia.
A non-selective beta-adrenergic agonist used primarily to treat bradycardia and heart block by increasing heart rate and contractility.