6 Junctional Arrhythmias
Junctional arrhythmias occur when the normal pacemaker, the SA node, is suppressed, when a block occurs in the conduction system, or when the AV node or bundle of His becomes irritable and takes over as the pacemaker of the heart. These rhythms originate from the AV node or the bundle of His. This results in a reverse or upward direction of impulse propagation, causing the atria to depolarize after the ventricles. Consequently, the P waves appear inverted or negative in the inferior leads (II, III, and aVF) on the 12-lead EKG, reflecting this retrograde atrial activation.
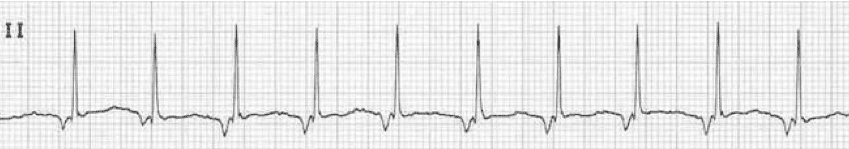
1. Premature Junctional Contractions
A premature junctional contraction (PJC) is a single premature beat arising from the AV node, interrupting the normal sinus rhythm and producing a narrow QRS complex, reflecting the normal conduction pathway through the bundle branches and Purkinje fibers. These are usually considered benign unless they occur frequently, which is typically defined as more than six PJCs per minute. Frequent PJCs indicate junctional irritability and may trigger more serious arrhythmias, such as junctional tachycardia. In patients taking digoxin, PJCs can be an early sign of toxicity.
Characteristics of PJCs
- Rhythm: Atrial and ventricular rhythms become irregular during PJCs, although the underlying rhythm may remain regular
- Rate: Depends on the underlying rhythm
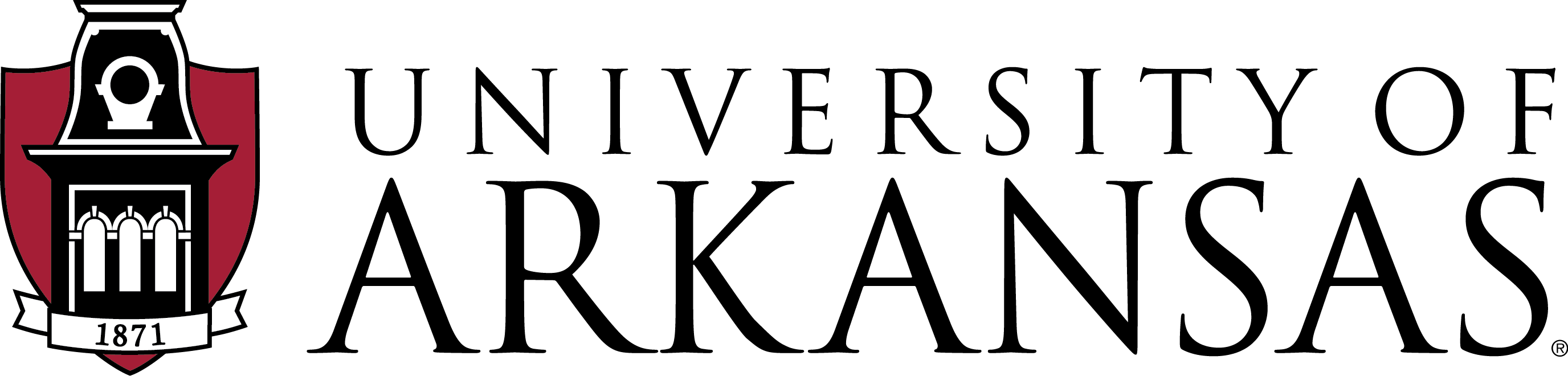
- P wave: Typically inverted, appearing before, during, or after the QRS complex. May be hidden within the QRS complex making it appear absent
- PR interval: When the P wave precedes the QRS complex, PR interval is shortened to less than 0.12 secs; otherwise, unmeasurable
Tolerance
- Most patients are asymptomatic with occasional PJCs
- Frequent PJCs may present palpitations, shortness of breath, fatigue, lightheadedness
- Sustained PJCs can potentially lead to junctional tachycardia, which may require treatment
Causes
- Underlying heart conditions like heart failure, coronary artery disease, cardiomyopathy, valvular heart disease
- Excessive caffeine, nicotine, or alcohol consumption
- Electrolyte imbalances
- Digitoxin toxicity
- Myocardial ischemia
- Hyperthyroidism
- Stimulant use
Treatment
- Generally aimed at the underlying cause
- Rate control with beta-blockers, calcium channel blockers
- Antiarrhythmic drugs may be used for rhythm control if difficult to treat
- Catheter ablation is rarely needed but may be considered for recurrent, symptomatic PJCs
- Lifestyle modifications (e.g., exercise, avoiding stimulants, etc.)
2. Junctional Escape Rhythm
When the SA node experiences dysfunction or its firing rate slows down significantly, the AV junction can take over as a secondary pacemaker. This can occur in situations such as:
- The SA node’s intrinsic rate dropping below the inherent rate of the AV junctional pacemaker cells, which typically ranges from 40–60 bpm
- Conduction blocks or delays preventing the SA node impulses from propagating effectively
- Impaired SA node function due to factors like ischemia, electrolyte disturbances, or autonomic influences
Under these circumstances, the AV junction assumes the role of generating electrical impulses to maintain cardiac activity, a phenomenon known as an “escape rhythm.” This escape mechanism allows the heart to continue beating, although at a slower rate, when the primary pacemaker fails or becomes suppressed, ensuring some measure of cardiac output is maintained.
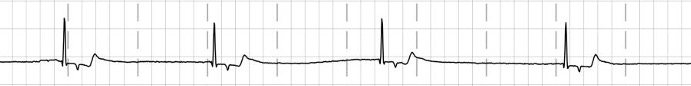
Characteristics of Junctional Escape Rhythm
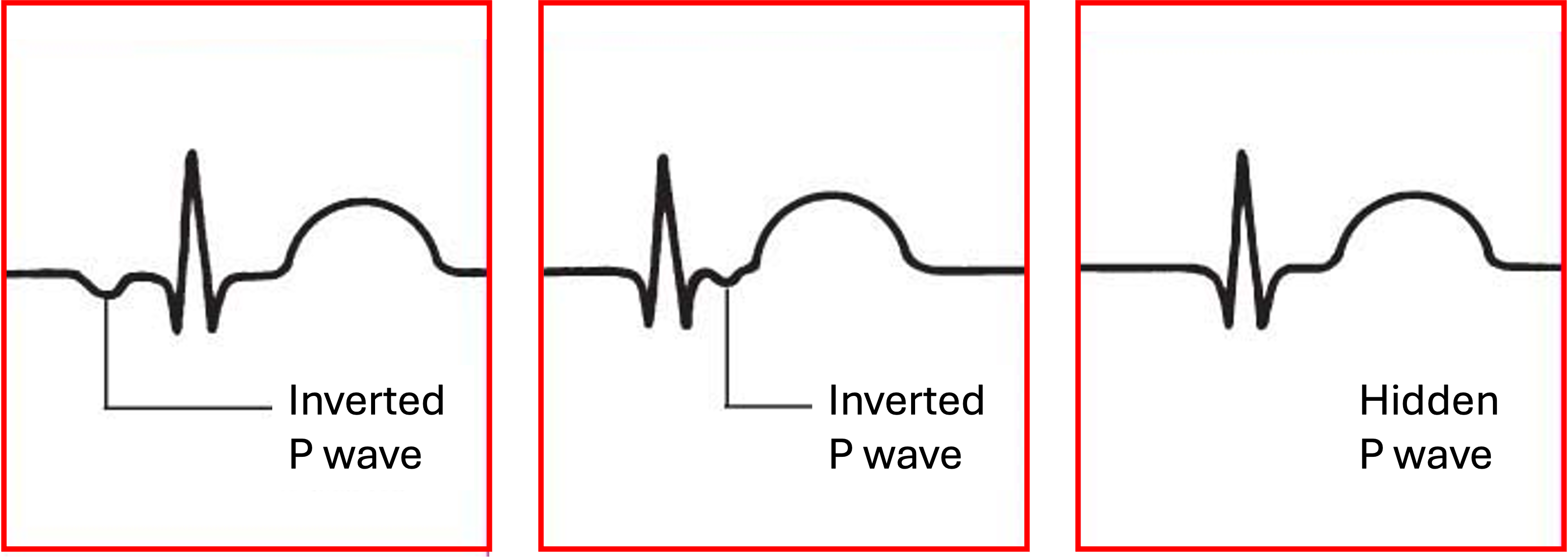
- Rhythm: Usually regular
- Rate: Ventricular rate typically between 40–60 bpm
- P wave: May be absent, inverted, or buried within the QRS complex
- PR interval: Usually short if P wave is present
- QRS complex: Typically narrow, unless an underlying conduction abnormality is present
- Tolerance: Often well-tolerated, unless there are prolonged episodes of bradycardia
Clinical Significance
- Often transient and may occur during sinus node dysfunction or after periods of sinus arrest
- Can be a normal physiological response to maintain cardiac output when the SA node fails
- However, persistent junctional escape rhythms may indicate underlying pathology or conduction system disease
Signs & Symptoms
- May be asymptomatic, especially with brief episodes
- Palpitations, dizziness, or lightheadedness can occur, especially with prolonged episodes
- May be more pronounced in patients with underlying heart disease
Treatment
- Often not required for brief, asymptomatic episodes
- Address the underlying cause
- Atropine or other chronotropic agents may be used to increase heart rate if bradycardia is severe
- Pacemaker implantation may be considered in cases of persistent or recurrent junctional escape rhythms with symptoms or hemodynamic compromise
Causes
- Sinus node dysfunction or sinus arrest due to various causes (e.g., ischemia, medications, electrolyte imbalances)
- Increased vagal tone or autonomic dysfunction
- Congenital or acquired conduction system abnormalities
- Digitoxin toxicity or other drugs that cause bradycardia
- Myocardial ischemia or infarction, myocarditis, pericarditis
- Chest trauma or cardiac surgery
3. Junctional Bradycardia
While a typical junctional escape rhythm has a rate between 40–60 bpm, junctional bradycardia is characterized by a heart rate below 40 bpm. This slower rate distinguishes it from the standard junctional escape rhythm and often indicates a more significant disruption of the heart’s normal pacemaker function. Junctional bradycardia can occur when there is suppression or failure of both the SA node and the AV junction’s usual escape rate, potentially leading to inadequate cardiac output and requiring closer monitoring or intervention.

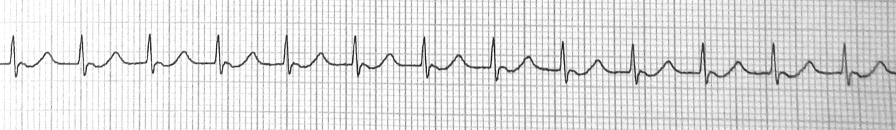
4. Accelerated Junctional Rhythm
Accelerated junctional rhythm is a cardiac arrhythmia originating from the AV junction, which serves as a backup pacemaker when the SA node fails to control the heart rate. It is characterized by a faster rate than the normal junctional escape rhythm but slower than junctional tachycardia. It often occurs when the SA node is suppressed or when the AV junction becomes more irritable and conducts automatic impulses.

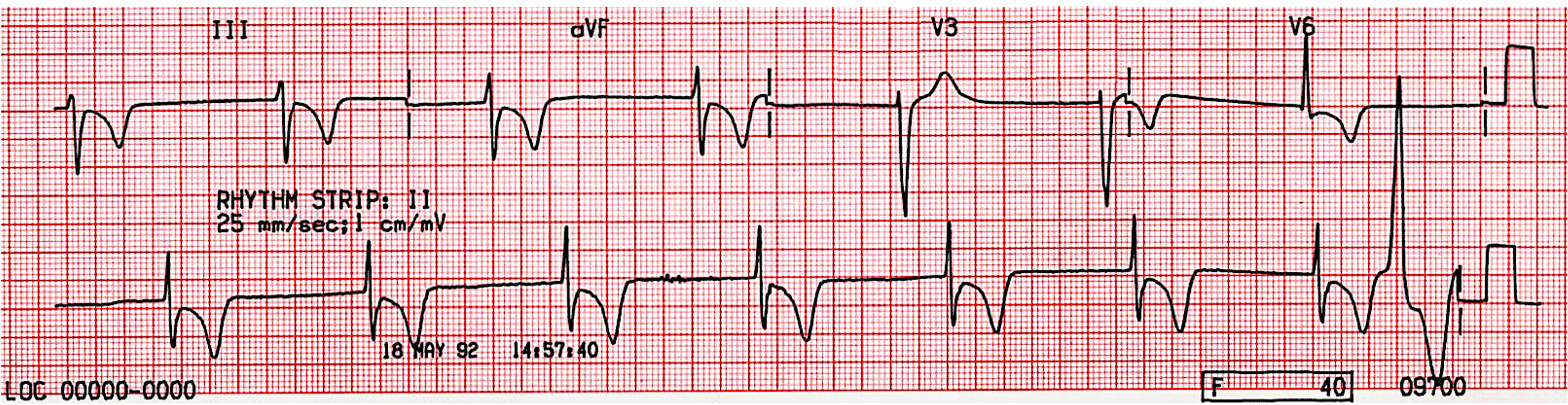
Characteristics of Accelerated Junctional Rhythm
- Rhythm: Usually regular
- Rate: Typically between 60–100 bpm
- P wave: May be absent, inverted, or occur after the QRS complex
- PR interval: Often not measurable due to P wave abnormalities
- QRS complex: Usually narrow (<0.12 secs) unless an underlying bundle branch block is present
- Tolerance: Generally well-tolerated due to adequate cardiac output. May cause mild symptoms in some patients
Clinical Significance
- Indicates suppression of the SA node or enhanced automaticity of the AV junction
- Often a transient rhythm that may resolve spontaneously
- Can be a sign of underlying cardiac or systemic issues
Signs & Symptoms
- Often asymptomatic
- Some patients may experience mild palpitations or fatigue
- Rarely causes significant hemodynamic instability
Treatment
- Usually does not require specific treatment if well-tolerated
- Address underlying causes (e.g., electrolyte imbalances, ischemia)
- In symptomatic cases, atropine or isoproterenol may be considered to increase heart rate
- Long-term management focuses on treating the underlying condition
Causes
- Acute myocardial infarction
- Digoxin toxicity
- Electrolyte imbalances, especially hypokalemia
- Elevated vagal tone
- Sick sinus syndrome
- Certain medications (e.g., beta-blockers, calcium channel blockers)
5. Junctional Tachycardia
When the AV junction is in control of the heart’s rhythm at a pace greater than accelerated junctional rhythm, it results in junctional tachycardia. Junctional tachycardia is a rare form of supraventricular tachycardia (SVT) characterized by a heart rate greater than 100 bpm, originating from a focus in or near the AV node. When the rate reaches or exceeds 150 bpm, any P waves present become more difficult to identify on the EKG.
Characteristics of Junctional Tachycardia
- Rhythm: Usually regular
- Rate: 100–250 bpm
- P wave: Often absent or retrograde (inverted in leads II, III, aVF). May occur before, during, or after the QRS complex
- PR interval: Variable or unmeasurable due to P wave abnormalities
- QRS complex: Typically narrow (<0.12 secs) unless there is a pre-existing bundle branch block
- Tolerance: Variable, depending on rate and underlying cardiac function. May cause hemodynamic instability at higher rates
Clinical Significance
- Indicates AV junction irritability or SA node dysfunction
- Can be a sign of underlying cardiac pathology or systemic illness
- May lead to hemodynamic compromise if sustained or at very high rates
Signs & Symptoms
- Palpitations
- Dizziness or lightheadedness
- Shortness of breath
- Chest discomfort
- Fatigue or weakness
Treatment
- Address underlying causes (e.g., correct electrolyte imbalances, treat ischemia)
- Vagal maneuvers or adenosine for acute termination
- Antiarrhythmic medications (e.g., beta-blockers, calcium channel blockers)
- In some cases, ablation may be considered
Causes
- Digitalis toxicity
- Myocardial ischemia or infarction
- Electrolyte imbalances
- Sympathetic stimulation (e.g., stress, caffeine, medications, stimulants)
- Congenital heart defects
- Post-cardiac surgery
Image Attributions:
Fig. 6.1 – This work, “Premature junctional contraction morphologies” is adapted from Junctional Arrhythmias by Dr. Zezo, used under CC BY-NC-SA 4.0. “Premature junctional contraction morphologies” is licensed under CC BY-NC 4.0 by Dr. Joshua E. McGee
Fig. 6.2 – This work is a derivate of “Junctional Escape Rhythm, Very Slow” by Dr. A Röschl and is licensed under CC BY-NC-SA 4.0
Fig. 6.3 – “Case B11. Junctional rhythm” by Simon Carley is licensed under CC BY-NC-SA 4.0
Fig. 6.4 – “Junctional escape rhythm” by Yassin, Subahu, Abubakar, Rashed, and Shokr in Wiley Online Library is licensed under CC BY 4.0
Fig. 6.5 – “ECG of the Week 1| answer” by Jason E. Roediger is licensed under CC BY-NC-SA 3.0 / Cropped from original
Fig. 6.6 – “Accelerated Junctional Rhythm” by Buttner and Burns is licensed under CC BY-NC-SA 4.0